Carotid stenting may be a safe alternative to endarterectomy in patients under age 70 years with symptomatic carotid stenosis, but stenting should be avoided in those aged 70 years or older, according to findings from a meta-analysis of data from three randomized controlled trials published online Sept. 10 in the Lancet.
While current recommendations restrict the use of stenting to symptomatic patients with contraindications to endarterectomy, carotid stenosis at surgically inaccessible sites, recurrent stenosis after previous endarterectomy, and stenosis after irradiation, the findings of this meta-analysis suggest stenting is also a viable alternative in younger patients in whom surgery could otherwise be undertaken without increased risk, said Dr. Leo H. Bonati of University Hospital Basel, Switzerland, and of the Institute of Neurology at University College, London, and his colleagues from the Carotid Stenting Trialists’ Collaboration.
They advised, however, that some uncertainty remains about whether recurrent stenosis rates are high after stenting vs. endarterectomy and recommended an approach of offering stenting when “technically feasible as an alternative option to endarterectomy to patients younger than 65-70 years with symptomatic carotid stenosis, in centers in which acceptable periprocedural outcomes have been independently verified ... as long as patients are made aware of a possible increase in the risk of restenosis.”
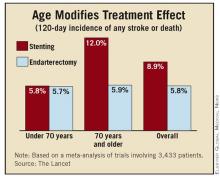
Among the 3,433 patients in the trials, the overall incidence of any stroke or death in the 120 days following randomization in the three trials was significantly greater in the patients who underwent carotid stenting vs. carotid endarterectomy (8.9% vs. 5.8%, respectively; risk ratio 1.53).
However, assessment of multiple subgroup variables showed that age modified the treatment effect; no difference was seen in the estimated 120-day risk of stroke or death in those under age 70 years who underwent stenting vs. endarterectomy (5.8% and 5.7%, respectively; risk ratio 1.00), but the risk of stroke or death was doubled in those aged 70 years or older who underwent stenting vs. endarterectomy (12.0% vs. 5.9%; risk ratio 2.04).
Similarly, the relative risk estimates for stroke or death at 30 days after treatment were comparable in those under age 70 years who underwent stenting vs. endarterectomy (5.1% and 4.5%, respectively; risk ratio 1.11), but were more than double in those aged 70 years or older for stenting vs. endarterectomy (10.5% and 4.4%, respectively; risk ratio 2.41).
The findings provide “strong evidence that, in the short term, the harm of stenting compared with endarterectomy decreases with younger age,” the investigators wrote.
For their meta-analysis, which was funded by the Stroke Association, the investigators analyzed pooled data from the Endarterectomy vs. Angioplasty in Patients With Symptomatic Severe Carotid Stenosis (EVA-3S) trial, the Stent-Protected Angioplasty vs. Carotid Endarterectomy (SPACE) trial, and the International Carotid Stenting Study (ICSS).
These and other trials have suggested there is a higher periprocedural risk of stroke with stenting vs. endarterectomy, but none of the trials on their own were sufficiently powered to show whether stenting might be a safe alternative in specific subgroups of patients, the investigators noted (Lancet 2010 Sept. 10 [doi:10.1016/S0140-6736(10)61009-4]).
Indeed, the risk of stenting remained strongly dependent on age even after additional assessment based on sex, type of recent symptoms, degree of treated carotid stenosis, systolic blood pressure at randomization, whether treatment occurred within 14 days of the most recent event, the number of patients recruited per center, the center recruitment rate, and history of diabetes, hypertension, hypercholesterolemia, smoking, coronary heart disease, peripheral artery disease, and prior stroke, the investigators noted.
“Age might represent a marker of the general burden of atherosclerosis of the aortic arch, or might be associated with increased plaque instability, altered configuration of the aortic arch, or vessel tortuosity. Hence, elderly patients might be at increased risk of dislodgement of plaque debris or thrombi during the stent procedures,” Dr. Bonati and his associates wrote.
In an update of an earlier systematic summary-data meta-analysis of randomized trials that compared endovascular treatment with endarterectomy for symptomatic carotid stenosis, the authors included recently released results from the Carotid Revascularization Endarterectomy vs. Stent Trial (CREST), among others, and found a short-term risk ratio of any stroke or death that was very similar to that seen in the current meta-analysis. This indicated that “the current findings are not biased by exclusion of previous trials and CREST,” noted the authors, who stated that they have no conflicts of interest.