An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
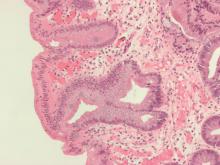
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.