The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported Jan. 25.
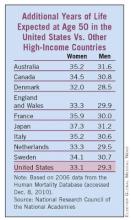
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States –the world’s top spender on health care -- fell below that of approximately nine other countries, including Australia, Japan, and Canada. (See graphic.)
The National Council on Aging commissioned the report, "Explaining Divergent Levels of Longevity in High-Income Countries," to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
"Smoking appears to be responsible for a good deal of the divergence in female life expectancy," according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20 to 30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%-35% of the difference in longevity between Americans and residents of countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The report was limited by a lack of markers to directly identify the impact on longevity of risk factors other than smoking, including obesity, physical inactivity, and stress, the researchers said.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.