After years of relative stability, firearm-related mortality in the United States rose sharply starting in 2015, according to analysis of a national mortality database.
U.S. firearm mortality was 10.4 per 100,000 person-years during 1999-2014, with the high in that period occurring in 2012 and dropping each of the next 2 years – compared with 11.8 per 100,000 during 2015-2017, an increase of 13.8%, Jason E. Goldstick, PhD, and associates wrote Oct. 8 in Health Affairs.
The majority of the 612,310 firearm deaths over the entire study period were suicides, with the proportion rising slightly from 58.6% in 1999-2014 to 60.0% in 2015-2017. Homicides made up 38.5% of deaths in 1999-2014 and 37.9% in 2015-2017, while the combined share of unintentional and undetermined deaths dropped from 2.9% to 2.1%, the investigators reported.
Dr. Goldstick of the University of Michigan, Ann Arbor, said in a separate written statement.
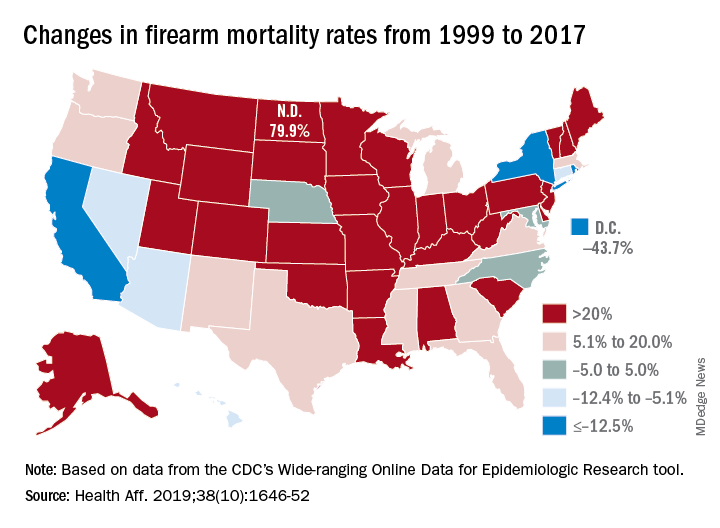
The geographic broadness can be seen when the change in mortality from 1999-2014 to 2015-2017 was calculated for each locale: 29 states had an increase of more than 20% and only 3 states (California, New York, and Rhode Island) and the District of Columbia had a decrease of at least 12.5%, they said. The data came from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research tool.
The different trends among states and subpopulations make it difficult to offer policy-based interventions. “The epidemiology of firearm violence is complex and varies based on the mechanism of death, demographic group under study, and regionally specific culture, making a one-size-fits-all solution inappropriate,” Dr. Goldstick and associates wrote.
The study was funded mainly by a grant from the National Institute of Child Health and Human Development. The investigators did not provide any information on conflicts of interest.
SOURCE: Goldstick JE et al. Health Aff. 2019;38(10):1646-52.