Coronavirus disease of 2019, more commonly referred to as COVID-19, is caused by a novel coronavirus. At press time in April, its diagnosis had been confirmed in more than 2 million individuals in 185 countries and territories since first isolated in January 2020. Daily updates are provided in terms of the number of new cases, the evolving strategies to mitigate additional spread, testing, potential drug trials, and vaccine development. Risk groups for development of severe disease also have been widely publicized. Limited information has been provided about COVID-19 in children.
Terminology
Endemic. The condition is present at a stable predictable rate in a community. The number observed is what is expected.
Outbreak. The number of cases is greater than what is expected in the area.
Epidemic. An outbreak that spreads over a larger geographical area.
Pandemic. An outbreak that has spread to multiple countries and /or continents.
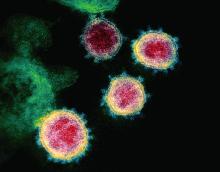
What we know about coronaviruses: They are host-specific RNA viruses widespread in bats, but found in many other species including humans. Previously, six species caused disease in humans. Four species: 229E, NL63, OC43, and HKU1 usually cause the common cold. Symptoms are generally self-limited and peak 3-4 days after onset. Infection rarely can be manifested as otitis media or a lower respiratory tract disease.
In February 2003, SARS-CoV, a novel coronavirus, was identified as the causative agent for an outbreak of a severe acute respiratory syndrome (SARS) which began in Guangdong, China. It became a pandemic that occurred between November 2002 and July 2003. More than 8,000 individuals from 26 countries were infected, and there were 774 deaths, according to the Centers for Disease Control and Prevention. No cases have been reported since April 2004. This virus most often infected adults, and the mortality rate was 10%. No pediatric deaths were reported. The virus was considered to have evolved from a bat CoV with civet cats as an intermediate host.
In September 2012, MERS-CoV (Middle East respiratory syndrome), another novel coronavirus also manifesting as a severe respiratory illness, was identified in Saudi Arabia. Current data suggests it evolved from a bat CoV using dromedary camels as an intermediate host. To date, more than 2,400 cases have been reported with a case fatality rate of approximately 35% (Emerg Infect Dis. 2020 Feb; 26[2]:191-8). Disease in children has been mild. Most cases have been identified in adult males with comorbidities and have been reported from Saudi Arabia (85%). To date, no sustained human-to-human transmission has been documented. However, limited nonsustained human-to-human transmission has occurred in health care settings.
Preliminary COVID-19 pediatric data
Multiple case reports and studies with limited numbers of patients have been quickly published, but limited data about children have been available. A large study by Wu et al. was released. Epidemiologic data were available for 72,314 cases (62% confirmed 22% suspected,15% diagnosed based on clinical symptoms). Only 965 (1.3%) cases occurred in persons under 19 years of age. There were no deaths reported in anyone younger than 9 years old. The authors indicated that 889 patients (1%) were asymptomatic, but the exact number of children in that group was not provided.1
Dong Y et al. reported on the epidemiologic characteristics of 2,135 children under 18 years who resided in or near an epidemic center. Data were obtained retrospectively; 34% (728) of the cases were confirmed and 66% (1,407) were suspected. In summary, 94 (4%) of all patients were asymptomatic, 1,088 (51%) had mild symptoms, and 826 (39%) had moderate symptoms at the time of diagnosis. The remaining 6% of patients (125) had severe/critical disease manifested by dyspnea and hypoxemia. Interestingly, more severe/critical cases were in the suspected group. Could another pathogen be the true etiology? Severity of illness was greatest for infants (11%). As of Feb. 8, 2020, only one child had died; he was 14 years old. This study supports the claim that COVID-19 disease in children is less severe than in adults.2
Data in U.S. children are now available. Between Feb. 12, 2020, and April 2, 2020, there were 149,770 cases of laboratory-confirmed COVID-19 reported to the CDC. Age was documented in 149,082 cases and 2, 572 (1.7%) were in persons younger than 18 years. New York had the highest percentage of reported pediatric cases at 33% from New York City, and 23% from the remainder of New York state; an additional 15% were from New Jersey and the remaining 29% of cases were from other areas. The median age was 11 years. Cases by age were 32% in teens aged 15-17 years; 27% in children aged 10-14 years; 15% in children aged 5-9 years; 11% in children aged 1-4 years; and 15% in children aged less than 1 year.
Exposure history was documented in 184 cases, of which 91% were household /community. Information regarding signs and symptoms were limited but not absent. Based on available data, 73% of children had fever, cough, or shortness of breath. When looked at independently, each of these symptoms occurred less frequently than in adults: 56% of children reported fever, 54% reported cough, and 13% reported shortness of breath, compared with 71%, 80%, and 43% of adults, respectively. Also reported less frequently were myalgia, headache, sore throat, and diarrhea.
Hospitalization status was available for 745 children, with 20% being hospitalized and 2% being admitted to the ICU. Children under 1 year accounted for most of the hospitalizations. Limited information about underlying conditions was provided. Among 345 cases, 23% had at least one underlying medical condition; the most common conditions were chronic lung disease including asthma (50%), cardiovascular disease (31%), and immunosuppression (8%). Three deaths were reported in this cohort of 2,135 children; however, the final cause of death is still under review.3
There are limitations to the data. Many of the answers needed to perform adequate analysis regarding symptoms, their duration and severity, risk factors, etc., were not available. Routine testing is not currently recommended, and current practices may influence the outcomes.
What have we learned? The data suggest that most ill children may not have cough, fever, or shortness of breath; symptoms which parents will be looking for prior to even seeking medical attention. These are the individuals who may likely play a continued role with disease transmission. The need for hospitalization and the severity of illness appears to be lower than in adults but not absent. Strategies to mitigate additional spread such as social distancing, wearing facial masks, and hand washing still are important and should be encouraged.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures. Email Dr. Word at pdnews@mdedge.com.
References
1. JAMA. 2020;323(13):1239-42.