Primary care clinicians, already experiencing all-time high stress levels related to COVID-19, are now struggling to cope with the fallout from racism and the death of George Floyd, according to a survey conducted June 5-8.
When asked how the situation has affected their practices, two-thirds of the survey’s 586 respondents said that George Floyd’s death and related events had been the subject of practice conversations and 12% “drew clear connections between the current racial unrest and the health of their patients,” the Larry A. Green Center said in a recent statement.
One-third of the clinicians also said that recent racism-related events have had a negative effect on their own well-being, and that connection was expressed even more strongly in a related survey of 1,111 patients that was conducted June 8.
In that survey, about 65% of patients said that racism affected emotional, psychological, and behavioral health, and 40% noted that George Floyd’s death had a negative impact on the well-being of friends, the Larry A. Green Center said in partnership with the Primary Care Collaborative and 3rd Conversation.
“The fact that so many patients and clinicians agree that racism is a driver of health points to the incredible role primary care plays in creating safe spaces to process deep societal and personal issues,” said Christine Bechtel, cofounder of 3rd Conversation, a community of patients and providers.
COVID-19, in the meantime, is still doing its thing. Almost two-thirds (63%) of respondents to the clinician survey said that stress levels at their practices had reached all-time-high levels in the last 4 weeks.
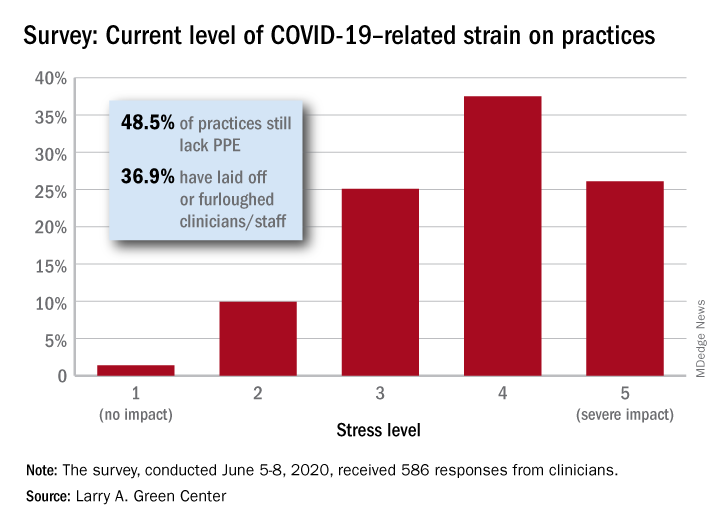
Just 1.4% of the primary care clinicians said that the pandemic had put no strain on their practices (see graph), and just 10% rated that strain as a 2 on a scale of 1-5, the center said. Among the stressors:
About 49% continue to lack PPE.
About 40% still have no or limited ability for testing.
About 37% of practice settings still report layoffs and furloughs.
About 31% report that clinician salaries are still being skipped or deferred.
“Both public and private policy makers must take immediate steps to stabilize primary care,” said Ann Greiner, president and CEO of the Primary Care Collaborative. “This financial support is necessary but not sufficient. Instead, we need wholesale reform of payment in order to achieve the kind of high-performing primary care that truly meets patient needs.”