What is the next step in treatment after a person with rheumatoid arthritis fails to adequately respond to methotrexate – a Janus kinase (JAK) inhibitor or a biologic? That was the focus of a lively debate at the virtual annual meeting of the American College of Rheumatology.
Vibeke Strand, MD, argued that JAK inhibitors offer the distinct advantage of a faster clinical response than biologics, meaning that decisions to change therapy based on nonresponse or adverse effects can be made earlier in a treatment plan.
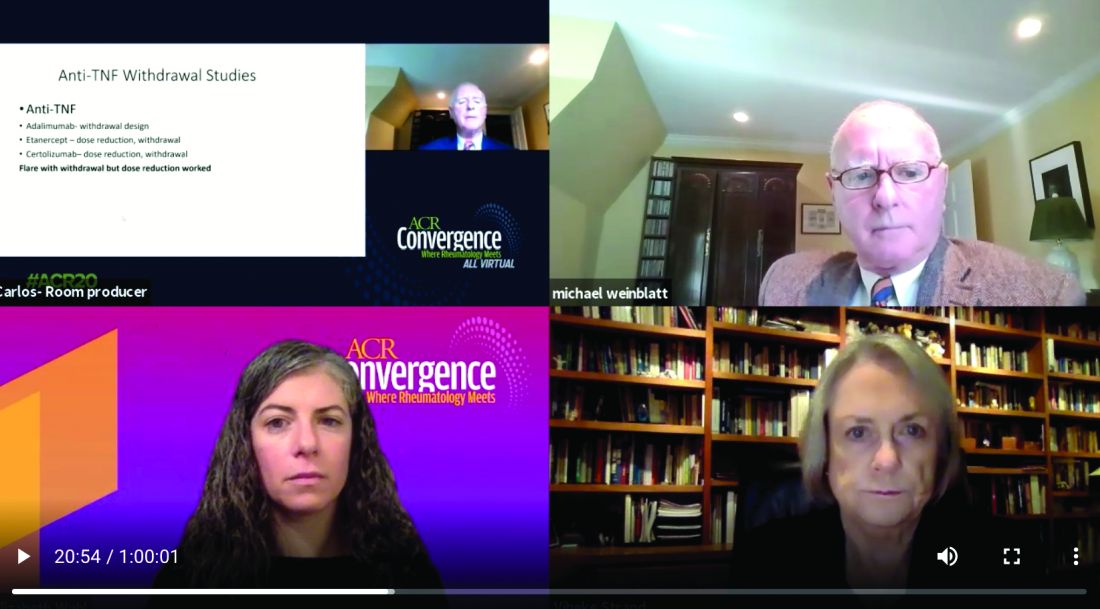
Michael Weinblatt, MD, countered that the faster-response advantage is offset by potential adverse events associated with the JAK inhibitors, including increased risk of herpes zoster infection, venous thromboembolism (VTE), and arterial thromboembolism (ATE). He suggested switching patients to a biologic instead.
In addition, the debate was held just days before the ACR released a proposed guideline for the management of RA. This update to the 2015 guidance is the first to prioritize the order of RA treatments, emphasizing that clinicians should maximize methotrexate therapy before switching RA patients to a JAK inhibitor or a biologic. Release of the full guidelines is pending, and it remains unclear if the ACR provides any guidance regarding the “jakinib” versus biologic decision.
Interestingly, the debate did not hinge on any differences in efficacy. Both speakers pointed to similar efficacy between anti–tumor necrosis factor (TNF) agents and JAK inhibitors, and despite working on different pathways, among the individual JAK inhibitors as well.
Is timing of the essence?
Knowing whether a person with RA responds to a JAK inhibitor more quickly than to a biologic is a major advantage, said Dr. Strand, of the division of immunology and rheumatology at Stanford (Calif.) University. “The argument that I am making is that patients are more responsive if treated earlier in the disease process and they are less treatment-experienced.”
Dr. Strand said the advantages extend to remission as well. “When patients are aware of early improvements, their adherence is increased. Remission is more likely because it occurs earlier.”
“I will certainly grant it to Vibeke that jakinibs work much faster,” said Dr. Weinblatt, chair of rheumatology at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School in Boston. However, he added, “my bias is that you give patients an anti-TNF therapy first, and if they are not responding by 12 weeks, you move on to another class of drugs, perhaps even the jakinibs.”
Herpes zoster risk
Dr. Strand and Dr. Weinblatt addressed potential adverse events associated with both classes of agents. For the JAK inhibitors, concerns include herpes zoster infections, increased VTE and ATE incidence, and largely unknown risks during pregnancy and lactation. For the anti-TNF agents, safety concerns include reactivation of tuberculosis, fungal infections, demyelinating syndrome, and skin cancer.
With the shortest half-life of any therapeutic class in rheumatology, adverse events with JAK inhibitors often can resolve quickly, Dr. Strand said.
The increased risk of herpes zoster is important, she added, “but we have a recombinant vaccination that works. It’s quite effective.”
Dr. Weinblatt pointed out that all the JAK inhibitors carry this increase herpes zoster risk, which is related to their mechanism of action. There is a catch with the vaccine, however, he added. The vaccine is approved for treatment of patients 50 years and older. For younger people with RA starting a JAK inhibitor, the cost is out-of-pocket.