Marine omega-3 fatty acids may be a promising add-on therapy for improving symptoms of borderline personality disorder (BPD), new research suggests.
A meta-analysis of four randomized controlled trials showed that adjunctive omega-3 fatty polyunsaturated fatty acids (PUFAs) significantly reduced overall BPD symptom severity, particularly affect dysregulation and impulsive behavior.
“Given the mechanisms of action and beneficial side effect profile, this [analysis] suggests that omega-3 fatty acids could be considered as add-on treatment” for patients with BPD, senior author Roel J. T. Mocking MD, PhD, resident in psychiatry and postdoctoral researcher at Academisch Medisch Centrum, Amsterdam, said in an interview.
The findings were published online in the Journal of Clinical Psychiatry.
Urgent need
“There are several effective treatments, but not all patients respond sufficiently,” which points to an urgent need for additional treatment options, Dr. Mocking said.
He noted that, although “several prior studies showed promising effects of omega-3 fatty acids” for patients with BPD, those studies were relatively small, which precluded more definitive overall conclusions.
The investigators wanted to combine results of the earlier studies to provide a combined estimate of overall effectiveness of the use of omega-3 fatty acids for patients with BP, with the intention of “guiding clinicians and individuals suffering from borderline personality disorder to decide on whether they should add omega-3 fatty acids to their treatment.”
The analyzed four studies that had a total of 137 patients. Three of the studies included patients diagnosed with BPD; one included individuals with recurrent self-harm, most of whom were also diagnosed with BPD.
Omega-3 fatty acids were used as monotherapy in one study. In the other studies, they were used as add-on therapy to other agents, such as antidepressants, benzodiazepines, and/or valproic acid. None of the studies included patients who were taking antipsychotics.
The type of omega-3 PUFAs were derived from marine rather than plant sources.
Three studies compared omega-3 fatty acids with placebo. One study compared valproic acid monotherapy with valproic acid plus omega-3 fatty acids and did not include a placebo group.
Significant symptom reduction
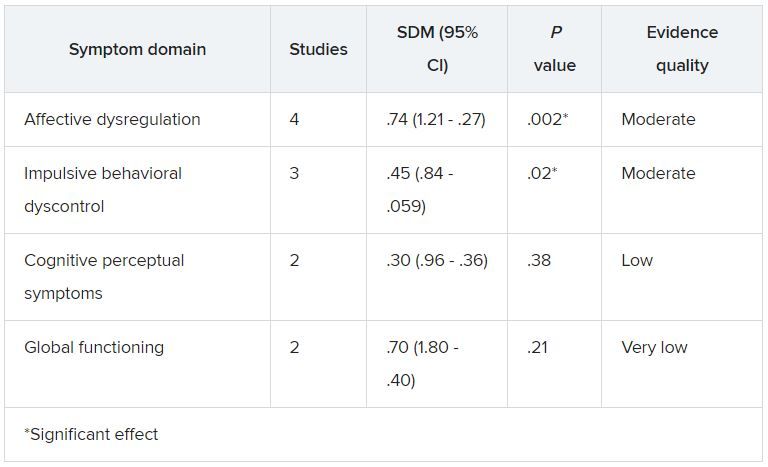
Random-effects meta-analyses showed an “overall significant decreasing effect” of omega-3 fatty acids on overall BPD symptom severity (standardized difference in means, 0.54; 95% CI, 0.91-0.17; P = .004) in the omega-3 group compared with the control group, with a medium effect size.
The investigators added that there was “no relevant heterogeneity” (P = .45).
Although heterogeneity was “more pronounced” in the affective dysregulation symptom domain, it did not reach statistical significance, the researchers noted.
The impulsive behavioral dyscontrol and cognitive perceptual symptom domains had “no relevant heterogeneity.” On the other hand, there was “substantial heterogeneity” in the global functioning symptom group.
Omega-3 fatty acids “have multiple bioactive roles in the brain. For example, they form essential components of the membrane of brain cells and thereby influence the structure and functioning of the brain. They also have an effect on inflammation levels in the brain,” Dr. Mocking said.
“Because we cannot synthesize these omega-3 fatty acids ourselves, we are dependent on our diet. The main dietary source of omega-3 fatty acids is fatty fish. However, since the industrial revolution, we eat less and less fatty fish, risking deficiency of omega-3 fatty acids causing brain dysfunction,” he added.
Dr. Mocking noted that
This “suggests that they could be combined to increase overall effectiveness,” he said.