Photo credit: Archives of Dermatology Feb. 21, 2011. doi:10.1001/archdermatol.2011.13. Copyright 2011 American Medical Association. All Rights Reserved.
Turns out that what had started as a mild drug reaction to a nonsteroidal anti-inflammatory drug had, within a short period of time, elevated to toxic epidermal necrolysis (TEN), a very dangerous and sometimes fatal condition. The woman had a bit of a circuitous route and several diagnoses before she ended up at the IU hospital.
She knew she had a history of NSAID sensitivity, and had gone to a tanning salon to self-treat the start of a rash which she rightly surmised came from ingesting ibuprofen. She was in the stand-up booth a short 8 minutes, and wore jeans, a bra, and eye shades. A few hours after tanning, she had increased itching, redness and pain, even in her throat. She went to the emergency department at her local hospital and was prescribed steroids and antibiotics for a suspected infection or drug reaction.
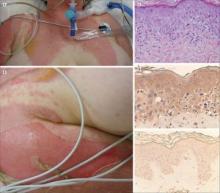
But within hours she had worsened; a return to the ED resulted in admission, and within a day, she was intubated. When she did not improve, she was transferred to IU. The dermatologists there suspected TEN. Skin biopsies "revealed a lymphocytic infiltrate at the dermoepidermal junction with some apoptotic keratinocytes consistent with TEN," noted the authors.
The young woman was treated in the burn unit, first with IV cyclosporine and supportive care. When things did not improve, she was given intravenous IgG. It was a week before she was extubated and 3 weeks before she went home.
That was not the end of the story, though. The IU team wanted to determine whether the radiation exposure from the tanning bed had led a mild drug reaction to become TEN. After a series of in vitro tests, the researchers determined that it appeared that "UV-A exposure in the setting of keratinocytes already activated from the pre-existing drug reaction resulted in an exaggerated production of epidermal cytokines such as [tumor necrosis factor]."
Many people — and some physicians — believe that tanning can help heal rashes or treat skin disease, reported the authors. But their study showed that rather than soothe or heal, the tanning bed radiation caused the skin to turn on itself in a toxic cascade.
— Alicia Ault (on Twitter @aliciaault)