LOS ANGELES – Several strokelike symptoms worked as strong risk factors for future strokes in patients with no history of strokes or transient ischemic attacks in a prospective study of more than 24,000 Americans.
"A history of strokelike symptoms appears to be a powerful risk factor for future stroke," Dr. Dawn O. Kleindorfer said at the International Stroke Conference. "Having any strokelike symptom was as predictive for future stroke as diabetes or atrial fibrillation. Having four or more strokelike symptoms is higher risk than any other risk factor."
Although these findings need confirmation and additional study, she envisioned eventually using these findings to create a new risk-factor screen for the general adult population.
People without a known history of stroke who have strokelike symptoms "are a group that hasn’t been well described before. They are at increased risk for stroke, but [today] they don’t get any kind of diagnosis. If we could design a way to ask questions that would predict the stroke risk in these patients, find them, and get them to medical care, we may help people at high stroke risk," said Dr. Kleindorfer, director of the division of vascular neurology at the University of Cincinnati. "This is not something to use yet; it needs more development. But eventually this could be part of general health assessment," she said in an interview.
Prior findings by Dr. Kleindorfer and her associates showed that 18% of Americans from the general public who had no known history of stroke or transient ischemic attack had at least one strokelike symptom either currently or in the past.
If the stroke-symptom questions undergo further validation, "we would have a way to be aggressive [in screening], like screening blood pressure. But this is even more powerful. It could be used at anything from public health fairs to assessing high-risk populations," commented Dr. Pooja Khatri, a neurologist and stroke specialist at the University of Cincinnati who has not been involved in this research.
The six questions ask about the sudden onset of painless hemibody weakness, painless hemibody numbness, difficulty understanding, difficulty speaking, loss of vision in one or both eyes, and loss of hemifield vision. These six questions derived from the Questionnaire for Verifying Stroke-Free Status (Stroke 2000;31:1076-80), Dr. Kleindorfer said in an interview.
The new study involved participants from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, which enrolled more than 30,000 white and African American U.S. residents, aged 45 years or older, during 2003-2007. The new analysis included 24,412 REGARDS enrollees, and excluded those who reported a history of stroke or transient ischemic attack. The researchers followed the study group for a median of 4.4 years, during which time this group had 381 incident strokes.
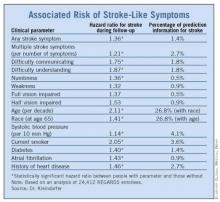
In an analysis that adjusted for the standard elements of the Framingham Stroke Risk Score, the researchers identified three strokelike symptoms significantly linked with an increased risk for incident stroke: Difficulty speaking, difficulty understanding, and numbness (see chart). These three symptoms each contributed approximately 2%, 2%, and 1%, respectively, of total stroke risk, making them at least as important to risk as diabetes and atrial fibrillation, which each contributed approximately 1% of total risk.
Each of the other three strokelike symptoms – weakness, half vision, and total vision impairment – did not individually have a statistically significant link to stroke incidence. However, collectively having a single strokelike symptom of any type increased a person’s relative risk for stroke by 36%, and represented more than 1% of total stroke risk. Among people with more than one strokelike symptom, each additional symptom increased stroke risk by a relative, statistically significant 21%, and overall multiple symptoms constituted nearly 3% of all stroke risk. These numbers meant that if a person had four strokelike symptoms, their relative risk of an incident stroke during 4.4 years of follow-up more than doubled, Dr. Kleindorfer said.
She noted her surprise that weakness was not a significant risk factor for later stroke. "I would have expected weakness to be the best predictor [of risk], but perhaps the people who suddenly couldn’t walk sought care and were diagnosed with stroke and were therefore excluded from the study," she said.
Dr. Kleindorfer also cautioned that the strokelike symptoms she studied could have resulted from causes other than a previously unrecognized stroke, such as seizure, syncope, migraine, psychiatric disease, ocular disease, low back pain, and dementia.
Dr. Kleindorfer said that she has been a consultant to Genentech and Boehringer Ingelheim. Dr. Khatri said that she had no disclosures.