It has also been difficult for his nurse, who is spending more time on data entry and less on interacting with patients, Dr. Machen said, adding that they are both in their late 50s and are more frustrated with the system than are their younger colleagues.
His staff has been happy; there’s no more searching for charts, and coding is easier, he said. And he does see the potential for improving quality, especially with the data-collection effort, warnings about drug interactions, and prompts for screening tests.
But for the time being, "it’s horrible with the workflow and the patient flow." On days of 15-20 patient visits, using the EHR is not as much of an issue. But on days of 30 patient visits, "it’s not doable," he said.
So far, patients haven’t been wild about the transition, either. They don’t like the physician to be working on a computer during the visit, he said. And "I don’t like it much, either," said Dr. Machen. "When I was in medical school, I was taught that the second you enter the exam room, the patient has your undivided attention." That’s not really possible with an EHR, at least the way he sees it currently, although he also can see possible solutions, such as having a scribe.
Dr. Machen also said he has concerns about whether it’s possible to truly secure an EHR, and, whether the systems will truly improve patient outcomes. The jury is still out on that, he said.
But, he added, "I don’t want to be a naysayer." He said that he’s "on the upward slope of the learning curve," and expects to get more comfortable eventually.
In September, he’ll begin his 90-day period of meaningful use, with the aim of receiving an incentive payment by the end of the year.
Medicare and Medicaid Incentives
The ONC provides the central leadership for the Medicare and Medicaid EHR incentive programs. The HITECH (Health Information Technology for Economic and Clinical Health) Act directly appropriated $2 billion to the ONC to spend on incentives and administration of the program. The federal regulation governing the incentive program (some 800 pages) was issued in July 2010.
This year – 2011 – is the first year in which physicians can participate; they have until Oct. 1 to attest that they are meaningful users. To be eligible for incentive payments, physicians have to meet the meaningful use criteria for 90 consecutive days.
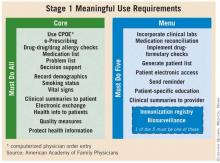
The criteria are being introduced in stages over the next 4-5 years. Stage 1 outlines what is expected in 2011 and 2012. Stage 2 was expected to be put into place in 2013, but in June, the Health IT Policy Committee of the Centers for Medicare and Medicaid Services voted to delay implementation until 2014, but only for physicians who were already participating. Physicians who wait until 2012 or later would still be expected to meet stage 2 criteria in 2013.
Physicians who want to participate have to choose between the Medicare or Medicaid incentive program. Those who take part in the Medicare program are eligible to receive incentive payments of $44,000 over 5 years. However, the payments will be made only through 2016. Physicians who wait until 2012 to start would still earn the $44,000 maximum; those who start later would receive prorated payments.
Physicians who practice in designated Health Professional Shortage Areas (HPSA) may be eligible for an additional 10% in each year’s incentive payment.
Importantly, Medicare begins to penalize nonparticipating physicians starting in 2016.
The Medicaid incentives are more generous: A total of $63,750 can be paid out over 6 years. And there’s a longer time frame. Eligible professionals can wait until 2016 to start participating and still receive the maximum payout over a 6-year period.
In late May, the CMS announced that $75 million in Medicare incentives had been awarded to physicians and hospitals in the first 2 weeks of the program. Some states began paying out Medicaid incentives in January. By late May, $83 million had been issued.
Meaningful use of EHRs is critical, according to Dr. Farzad Mostashari, the National Coordinator, who testified to the House Small Business Committee’s Subcommittee on Healthcare and Technology in June.
"If all we do is put an EHR in every provider’s office or hospital, we will have failed to realize health IT’s full potential," he said. "Instead, doctors, hospitals, and other providers need to use robust EHR technology in a meaningful and interoperable way to improve care."