HOUSTON – Repeat bronchoalveolar lavage should be considered for tailoring the duration of antibiotic therapy and for reassessing resistance profiles in patients with ventilator-associated pneumonia from infection with non–lactose fermenting gram-negative bacilli.
New clinical evidence endorses prolonged antibiotic therapy in these patients. Importantly, the findings also indicate that these patients have persistent primary infections, rather than recurrent infections, as has been previously suggested, Dr. Gina R. Shirah reported at Annual Congress of the Society for Critical Care Medicine.
The distinction between persistent and recurrent infection is important, she emphasized, as the former may signal drug resistance in some patients. For this reason, repeat bronchoalveolar lavage (BAL) should be considered during therapy, both to tailor duration of antibiotics and reassess for changes in resistance profiles.
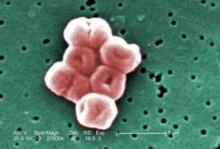
The American Thoracic Society recommends an 8-day antimicrobial treatment protocol for ventilator-associated pneumonia (VAP) but advises a longer course of therapy in patients with non–lactose fermenting gram-negative rods (NLF-GNR), which include Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia (Am. J. Respir. Crit. Care Med. 2005;171:388-416). The recommendation is based on the findings of a pioneering randomized study by the PneumA Trial Group that showed 8-day treatment to be as effective as 15-day treatment except in a subgroup of patients with NLF-GNR, in whom they observed higher recurrence rates (JAMA 2003;290:2588-98).
Dr. Shirah and her fellow researchers at the Maricopa Integrated Health System in Phoenix, including lead investigator Dr. Tammy Kopelman, conducted a study that indicates 8-day antibiotic regimens were associated with persistent primary infections, not recurrent infections, in patients with gram-negative bacilli.
The researchers retrospectively studied patients at a level I trauma center admitted over a 4½-year time period. They examined data for all ventilator-associated pneumonia patients who were diagnosed via bronchoalveolar lavage – and who underwent subsequent BAL during the antimicrobial treatment course. Based upon initial BAL pathogen, the patients were classified into two groups: those with NLF-GNR and those with all other pathogens, including Enterobacteriaceae, methicillin-resistant Staphylococcus aureus, and community-acquired Haemophilus spp, methicillin-sensitive S. aureus, and Streptococcus spp. They were then further divided based on whether the repeat BAL was conducted within fewer than 8 days of appropriate antibiotic therapy or at day 8 or later, Dr. Shirah said. "Persistent primary infection was defined as a less than 2-log 10 decrease of the initial species on subsequent bronchoalveolar lavage," she explained.
Of the 77 surgical intensive care unit patients who met the study criteria, 99% received appropriate empiric therapy, said Dr. Shirah. The average subsequent BAL performance was on day 7 (range, 3-14 days), with 37 patients undergoing the procedure after 8 days of therapy; of those, 13 patients were in the NLF-GNR group. Within that group, persistent primary infection after more than 8 days of appropriate antimicrobial therapy was reported in nine of the patients (69%) – seven with P. aeruginosa and two with A. baumannii.
By comparison, only two patients in the second group (8%) – both with Enterobacteriaceae – had evidence of persistent primary infection, representing a statistically significant difference, she said. "Importantly, in the [NLF-GNB] group, 56% of the pathogens obtained on repeat BAL remained sensitive to the treatment antibiotics, so nearly half of the patients required alternative antibiotic treatment."
The investigators also sought to determine whether persistent infection could have been predicted. They separated patients into three groups based on treatment status: treated (microbiologic cure on subsequent BAL); persistently infected antimicrobial sensitive; and persistently infected antimicrobial resistant. A comparison of clinical parameters across the groups showed that although there was some variation in white blood cell count, temperature, and ventilator needs "none of the differences were statistically significant," and thus not predictive of short-course treatment success or persistent infection, Dr. Shirah said.
The data strongly support the conclusion that a shortened course of antibiotics in patients with VAP caused by NLF-GNR will frequently lead to a persistent primary infection, said Dr. Shirah, noting that, in the case of NLF-GNR, "changes in antibiotic profiles are common and without reliable clinical indicators." For this reason, she stressed, repeat BAL should be considered during therapy, both to tailor duration of antibiotics and to reassess for changes in resistance profiles.
"Eight days is simply not enough," Dr. Shirah said.
On behalf of her coinvestigators and herself, Dr. Shirah reported no conflicts of interest with respect to this study.