CHICAGO – Bariatric surgery crushed intensive medical therapy for the management of hyperglycemia in a randomized trial involving obese patients with poorly controlled type 2 diabetes.
"The lesson of this study is that for those obese patients who also have uncontrolled diabetes, there is now another treatment option that may be very, very effective at getting them in good control," Dr. Philip R. Schauer declared in presenting the 1-year results of the STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) trial.
STAMPEDE was a single-center prospective study involving 150 randomized patients. The primary end point – hemoglobin A1c of 6.0% or less at 1 year – was achieved in 42% of patients in the Roux-en-Y gastric bypass group, 37% in the sleeve gastrectomy group, and 12% of patients assigned to state-of-the-art intensive medical management based upon American Diabetes Association guidelines, including a weight loss program, reported Dr. Schauer, professor of surgery and director of the Bariatric and Metabolic Institute at the Cleveland Clinic.
At enrollment the average HbA1c was 9.2% even though most patients were on three or more diabetes medications, and about half were taking insulin. The average baseline body mass index was 37 kg/m2. More than 60% of subjects had moderate to severe fatty liver disease.
Particularly noteworthy was the finding that all gastric bypass patients with an HbA1c of 6.0% or less at 1 year achieved that target despite having discontinued all diabetes medications, including insulin. So did 13 of 18 patients in the sleeve gastrectomy group who reached the primary end point.
"That’s as close to a definition of remission of diabetes as you can get to," the surgeon commented.
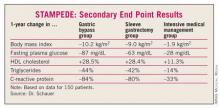
Improvements in secondary study end points related to cardiovascular risk were also far more impressive in the surgery arms.
Three patients in the gastric bypass group and one in the sleeve gastrectomy arm required redo operations. There were other serious complications in the surgical groups as well, but no deaths.
Follow-up of STAMPEDE participants will continue through 4 years. Dr. Schauer predicted that on the basis of the highly positive STAMPEDE findings, future studies will look at bariatric surgery versus intensive medical management in obese type 2 diabetic patients with lesser degrees of uncontrolled type 2 diabetes – say, HbA1cs between 7% and 9%.
Reaction to STAMPEDE was cautious.
"That’s a huge intervention in order to get control of diabetes. I’m just not sure it’s ready for prime time yet," former ACC President Dr. W. Douglas Weaver said in an interview.
"I would like to see some more outcomes data in patients who’ve been managed in this way. You’d like to see that it not only keeps the weight off and the glucose levels lower over the longer term, but that it actually improves outcomes in terms of cardiovascular events and diabetic complications. Then it becomes compelling. Right now, we just have these surrogate improvements," added Dr. Weaver, head of the division of cardiovascular medicine at the Henry Ford Health System, Detroit.
Cleveland Clinic endocrinologist Dr. Sangeeta Kashyap, who headed the STAMPEDE diabetology team, said medical therapy is not to be discounted. It’s titratable, even stoppable if need be. A surgical fix is not.
"Surgery works very well, but once it’s done, it’s done. If you want to eat an extra bite of food, you’re not going to be able to without getting violently ill," she observed in an interview.
"Even though our results strongly support bariatric surgery for diabetes, I don’t think it’s going to be right for everybody. I think more studies need to be done to figure out who the best candidates are, and for which procedures," Dr. Kashyap said.
The durability of surgery’s antidiabetic effect has yet to be established, she added.
Simultaneously with Dr. Schauer’s presentation of STAMPEDE in Chicago, the study was published online by the New England Journal of Medicine (N. Engl. J. Med. 2012 March 26 [10.1056/NEJMoa1200225]).
STAMPEDE was supported by Ethicon Endo-Surgery, the National Institutes of Health, and LifeScan. Dr. Schauer and Dr. Kashyap reported serving as consultants to Ethicon, and Dr. Schauer consults for other companies as well.