NEW ORLEANS – A five-session hypnosis program reduced the frequency and severity of postmenopausal hot flashes by 80%, according to the results of a randomized controlled trial presented at the annual meeting of the Society of Behavioral Medicine.
"It appears that hypnosis, when properly applied, can be a safe and effective treatment for hot flashes. And side benefits appear likely. We had a lot of women comment that they were generally feeling better; improvement in sleep was a big deal," Gary Elkins, Ph.D., said in presenting the results at the meeting. This trial was honored by the society as the outstanding study in the field of complementary and alternative medicine during the past year.
Dr. Elkins and his colleagues randomized 184 postmenopausal women with moderate to severe hot flashes to either five weekly hypnosis sessions or a structured attention control condition of equal duration.
Hot flash frequency and severity scores as recorded in patients’ daily hot flash diaries fell by about 70% at 5 weeks and even further to 80% at 12 weeks of follow-up, 7 weeks after the intervention ended, reported Dr. Elkins, professor of psychology and neuroscience at Baylor University in Waco, Tex.
Another key study end point was change in physiologically measured hot flashes obtained via a 24-hour skin conductance monitor sensitive to sweating; this tool was particularly helpful in getting objective data on nighttime hot flashes. Hot flashes as documented by the monitor, the Biologic HF Recorder with computer linkage, declined by about 50% at 5 weeks and 60% at 12 weeks. In contrast, the control group showed a 10% decrease in hot flashes at 5 weeks and a 15% reduction at 12 weeks.
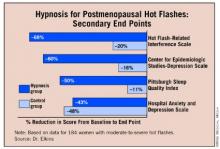
Secondary end points assessing sleep, depression, and hot flash–related interference with daily life also showed marked improvement in the hypnosis group.
The intervention entailed hypnotic induction with relaxation and direct and indirect suggestions, dissociation, and mental imagery evoking coolness, such as walking down a mountain path on a cool day. The imagery was individualized to incorporate places a patient had been and things she’d experienced. The emphasis was on teaching patients self-hypnosis with the goal of patient empowerment, the psychologist explained.
Results with the hypnosis intervention compare favorably with studies of other proposed treatments for hot flashes. For instance, the nonpharmacologic therapies black cohosh, soy, and vitamin E have been shown "virtually indistinguishable" from placebo, according to Dr. Elkins.
Venlafaxine and SSRIs have achieved roughly a 50% reduction in hot flashes in clinical trials. While that’s a clinically meaningful improvement, it’s a weaker effect than seen in the hypnosis trial. Moreover, Dr. Elkins noted, some women don’t want to take drugs or they experience limiting side effects. Hormone replacement therapy, formerly the standard treatment for hot flashes, has fallen into disfavor since the 16,000-subject Women’s Health Initiative was halted early due to a 26% increase in breast cancer, a 29% increase in coronary heart disease, and a 41% greater risk of stroke than in the placebo arm (JAMA 2004; 29:1701-12).
The critical next step in this hypnosis research project is to disseminate the required therapeutic skills as widely as possible. After all, it’s estimated that more than 25 million American women experience hot flashes, and 4 million of them are severely affected.
"I think we’ve shown this is a very effective therapy, but we need to find a way to make it widely available," the researcher observed.
He and his coinvestigators are pursuing a twofold dissemination strategy. They are developing a treatment manual for interested health care professionals, although "that’s still not going to create an army of practitioners," Dr. Elkins noted. So in addition, the investigators plan to put a guided hypnotic intervention on a CD for self-treatment.
"That could be very widely distributed. Even if it’s not quite as effective, I think that’s going to be the long-term way to go," according to the psychologist.
In an earlier, smaller randomized trial, Dr. Elkins showed that hypnosis also was highly effective in reducing hot flashes in breast cancer survivors on hormone-suppressing therapy (J. Clin. Oncol. 2008;26:5022-6). Unlike the new study in women with postmenopausal hot flashes, however, the study in breast cancer patients relied solely on patient self-reported symptoms without physiologic monitoring.
The trial was funded by the National Institutes of Health’s National Center for Complementary and Alternative Medicine. Dr. Elkins and his colleagues reported having no financial conflict.