It’s a scenario with which hospitalists are quite familiar: Mrs. A is discharged from the hospital to a skilled nursing facility on a Friday night. On Saturday, she develops a deep cough and fever, but the nursing facility’s attending physician isn’t scheduled to round until Monday. So Mrs. A ends up back in the hospital.
Such a readmission could have been prevented – and now that Medicare’s readmission penalties are about to kick in, more hospitalists are investigating systems and models to help them improve their readmission rates.
Under the Affordable Care Act, Medicare will begin on Oct. 1 to penalize hospitals with excess readmission for pneumonia, heart failure, and myocardial infarction – up to 1% of their overall Medicare payments, the Centers for Medicare and Medicaid Services recently announced. The penalty for this fiscal year (Oct. 1, 2012–Sept. 30, 2013) is based on hospital performance between July 2008 and June 2011, and is adjusted per hospital based on patient demographics, comorbidities, and frailty.
So, what’s a hospitalist to do to help lower the penalty going forward?
Focus on Skilled Nursing Facilities
Readmissions such as Mrs. A’s could be prevented if physicians had a stronger presence at the skilled nursing facility (SNF) level, according to Dr. Darius K. Joshi of the University of Michigan, Ann Arbor.
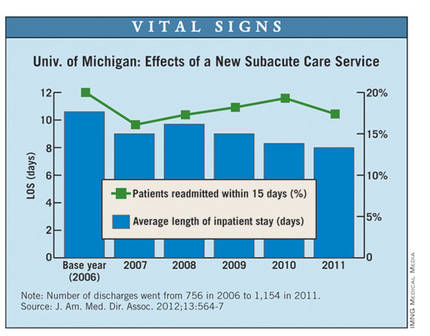
At the University of Michigan Health System, a small team of geriatricians and nurse practitioners, led by Dr. Joshi, has been assigned to staff local SNFs 7 days a week. The goal is to discharge patients from the hospital to SNFs sooner and to keep them from being readmitted.
The subacute care program reduced the average hospital length of stay before transfer to an SNF from 10.6 days to 8 days between 2006 and 2011. The hospital’s 15-day readmission rates have also improved somewhat, dropping from 20% to 17% over the same period (J. Am. Med. Dir. Assoc. 2012;13:564-7).
"Being at the bedside, seeing these patients, knowing their history, having good laboratory tests available, avoids sending many of these patients back to the hospital," said Dr. Joshi of the geriatric medicine division at the University of Michigan, a former hospitalist who runs the subacute program.
Doctors and nurse practitioners practicing in the SNFs also have access to the health system’s electronic health record (EHR) system. This allows physicians at the SNF to understand the patient’s hospital care; it also transfers data on care provided at the SNF back to the hospital.
But even with this effort, the University of Michigan health system (which has invested in ways to prevent bounce-back to the hospital) will face a 0.64% cut under the Hospital Readmissions Reduction Program in FY 2013.
"[Readmissions are] a very, very resistant problem with our patients," Dr. Joshi explained.
Many times, families may insist that their loved ones go to the emergency department when their conditions worsen. In the case of falls, there is little alternative to returning to the hospital because most SNFs don’t have appropriate imaging equipment.
"There are limitations in what we can do, but if there’s any chance of cutting down readmissions, it needs to be with bedside presence," Dr. Joshi said.
Multidisciplinary Approach
At Sarasota (Fla.) Memorial Hospital, one focus in the fight to lower readmission rates is on heart failure.
The hospital established a heart failure center for ambulatory patients and instituted telemonitoring for nonambulatory patients who are discharged to home. A team of hospitalists, cardiologists, floor nurses, and home health care staff identifies high-risk heart failure patients, addresses their needs in the hospital, and arranges for follow-up care after discharge.
Sarasota Memorial Hospital is considered a standout when it comes to keeping readmission rates low. It was one of only two hospitals identified by CMS as having better-than-average readmission rates for all three assessed conditions.
The lion’s share of the credit for their success goes to the multidisciplinary culture of the health system, according to Dr. John Moritz, a hospitalist at Sarasota Memorial.
"Communication and teamwork are key," Dr. Moritz said. "Our whole culture is characterized by working with the other staff members to ensure a favorable outcome for our patients."
This fall, Sarasota Memorial will take that approach a step further. They have dedicated two hospital floors to multidisciplinary rounds, where hospitalists, case managers, social workers, heart failure nurses, and physical therapists will round as a group.
"During that visit, we’ll be able to identify what’s needed," Dr. Moritz said. "We’ll be able to clearly communicate that to the patient and to each other."