The prevalence of nonrefractive visual impairment rose 21% in the general U.S. adult population during the most recent decade for which statistics are available, and that increase may be related to the recent rise in the rate of diabetes, according to a report in the Dec. 12 issue of JAMA.
In what they described as the first study to have noted this increase in the visual disorder, researchers found that the overall prevalence of nonrefractive impairment among adults in the United States rose from 1.4% in 1999-2002 to 1.7% in 2005-2008.
Notably, the largest absolute increase occurred in the youngest adults, those aged 20-39 years, across all racial and ethnic groups. The elevation also was particularly large among Mexican Americans aged 60 and older, among whom it rose from 4.6% to 8.9%, said Dr. Fang Ko of the Dana Center for Preventive Ophthalmology, Johns Hopkins University, Baltimore, and her associates.
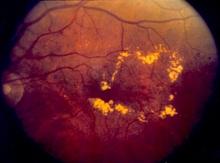
Nonrefractive visual impairment refers to a presumably organic eye disorder that impairs vision and cannot be corrected with eyeglasses. The most common causes are age-related macular degeneration, cataracts, diabetic retinopathy, and glaucoma.
Dr. Ko and her colleagues hypothesized that the prevalence of nonrefractive visual impairment may be increasing along with the increasing prevalence of diagnosed diabetes that has been reported in the literature. Rates of any type of diabetes rose from 4.9% in 1990 to 6.5% in 1998, 7.9% in 2001, 10.7% in 2007, and 11.3% in 2010, according to epidemiologic studies.
The investigators analyzed data from the National Health and Nutrition Examination Surveys (NHANES) to compare the prevalence of nonrefractive visual impairment in U.S. adults during 1999-2002 with that during 2005-2008. Conducted by the National Center for Health Statistics, NHANES examines health-related issues in nationally representative samples of approximately 10,000 adults every 2 years.
Participants in NHANES undergo extensive physical examinations that include vision assessments. A total of 8,790 adults completed a visual acuity exam during the first study period and 9,762 did so during the second study period.
The prevalence of nonrefractive visual impairment rose from 1.4% in 1999-2002 to 1.7% in 2005-2008, a relative increase of 21%.
In a multivariate analysis, factors that were associated with the visual disorder were older age, poverty, lower educational status, and diabetes. The only one of these risk factors that increased during the study periods was diabetes. In this study population, the overall prevalence of diabetes increased from 6.5% in 1999-2002 to 8.2% in 2005-2008, and the prevalence of diabetes of at least 10 years’ duration rose from 2.8% to 3.6%.
"Other than diabetes, we were unable to identify any other reason for increasing prevalence of nonrefractive visual impairment," Dr. Ko and her associates wrote (JAMA 2012;308:2361-8).
In study subjects who didn’t have diabetes, the prevalence of nonrefractive visual impairment was 1.2% in 1999-2002 and 1.4% in 2005-2008. In contrast, the prevalence of this type of visual impairment among subjects with diabetes was 3.7% in the first study period and 5.3% in the second.
In addition, the prevalence of nonrefractive visual impairment increased with increasing duration of diabetes.
And in an additional analysis of the data, controlling for diabetes status eliminated the difference in the prevalence of nonrefractive visual impairment between the two study periods.
The largest absolute increase in the prevalence of the eye disorder occurred in the youngest adults, which "is consistent with the hypothesis that increasing prevalence of diabetes among younger U.S. residents, with subsequent increasing duration of diabetes, may be related to worsening vision," the investigators said.
If the study findings are confirmed and this trend persists, "it could result in increasing rates of disability in the U.S. population, including greater numbers of patients with end-organ diabetic damage who would require ophthalmic care," they added.
This study was supported by the Centers for Disease Control and Prevention and the David Friedman Research Grant Award. Dr. Ko reported receiving a grant from Pepose, and one of his associates reported ties to several makers of ophthalmologic products.