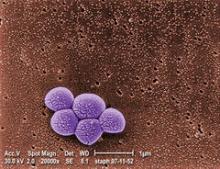
A universal decolonization strategy reduced the risk of methicillin-resistant Staphylococcus aureus infections by 37% in intensive care units – a significant improvement over the recommended strategy of targeting only carriers.
The protocol was easy – daily intranasal mupirocin and chlorhexidine skin washing – and cheap, with a total cost of about US$40 per patient, Dr. Susan S. Huang and her colleagues wrote in the May 29 issue of the New England Journal of Medicine.
But the finding should also be viewed with a note of caution, wrote Dr. Huang of the University of California Irvine.
"Widespread use of chlorhexidine and mupirocin could possibly engender resistance," which has been reported in some prior studies of MRSA decolonization," she noted. A MRSA gene conferring chlorhexidine resistance has been found, but it’s still unclear whether it is clinically significant. "It will therefore be important for surveillance programs to monitor mupirocin and chlorhexidine resistance" (N. Engl. J. Med. 2013 [doi:10.1056/NEJMoa1207290])
The team studied three protocols designed to tamp down nosocomial MRSA infections: MRSA screening with isolation for positive patients; targeted isolation, with screening, isolating, and decolonizing of patients with MRSA; and universal decolonization of all patients.
The universal approach does not incorporate screening. Instead, commencing with admission to the ICU, every patient receives twice-daily intranasal mupirocin for 5 days and daily bathing with chlorhexidine-impregnated cloths for the entire ICU stay.
The study’s primary outcome was ICU-attributable MRSA positive cultures. Secondary outcomes were ICU-attributable MRSA bloodstream infections, and bloodstream infections caused by any other pathogen.
The authors randomized 43 hospitals (comprising 74 ICUs) to the protocols, which were employed in a total of 74,256 patients. These were a median of 65 years, with a variety of coexisting conditions, including diabetes (about 31%), renal failure (about 20%), cancer (about 11%), and liver failure (about 4%). About 10% had a past history of MRSA infection. The median ICU stay was 3 days, and the median hospital stay, 7 days.
The risk analysis compared each hospital’s results with its own baseline data. Universal decolonization was the most effective means of preventing MRSA-positive cultures, significantly reducing the risk of a MRSA-positive culture by 37% (odds ratio, 0.63). This result was significantly better than either the targeted screening protocol, which reduced the risk by 25% (OR, 0.75) or the screening/isolation protocol, which reduced the risk by 8% (OR 0.92).
There were no significant differences in the risk of MRSA bloodstream infections in any of the groups. However, the authors noted, universal decolonization was associated with a greater reduction than either screening/isolation or targeted decolonization’s (OR, 0.74 vs. 1.20 and 1.19, respectively).
Both universal and targeted decolonization significantly reduced the risk of a bloodstream infection caused by any pathogen (OR, 0.55 and 0.77, respectively). Screening/isolation did not significantly affect this outcome (OR, 0.98).
There were seven adverse events – two in the targeted decolonization and five in the targeted decolonization groups. All of these were skin reactions to the chlorhexidine bath and resolved when that was discontinued.
Although the authors said the intervention was inexpensive, they recommended a more-detailed cost analysis. Such a study would examine the US$40 per patient cost in light of cost reductions associated with cessation of screening, reduced isolation precautions, and reduced infections, and of the potentially increased costs associated with any emergence of resistant MRSA strains.
"It remains to be seen whether universal decolonization can obviate the need for all contact precautions for carriers of MRSA or other multidrug-resistant organisms," they added.
The study was funded by the U.S. Agency for Healthcare Research and Quality and the U.S. Centers for Disease Control and Prevention. Dr. Huang did not report having any financial disclosures, but several of the coauthors stated they had financial ties with Sage Products and Express Scripts.