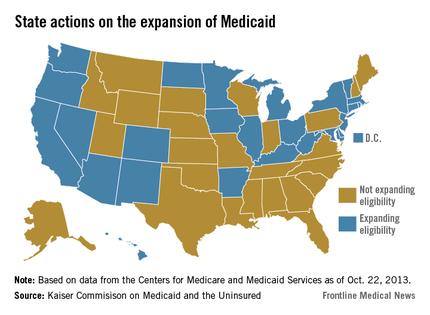
When the Supreme Court upheld the constitutionality of the Affordable Care Act in 2012, it also ruled that states could choose whether to substantially expand their Medicaid programs. That decision has created a split across the country, with about half of the states choosing to take federal dollars to expand their programs and the others opting out.
There’s no deadline on Medicaid expansion, so those states that have opted out so far can always choose to expand at a later date.
Here’s a look at two bellwether states: California, which has accepted federal money to expand its Medi-Cal program, and Texas, which has opted out of the expansion.
California Gov. Jerry Brown (D), a strong supporter of the ACA, announced that his state would expand Medicaid to include low-income individuals up to 138% of the federal poverty level starting on Jan. 1, 2014. All of the new enrollees – likely 1 million Californians – will be added to the state’s growing Medicaid managed care program.
Conversely, Texas Gov. Rick Perry (R) deemed Medicaid expansion "a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare."
California: Pay cuts complicate expansion
Physicians in California are bracing for a significant Medicaid pay cut at the same time as about a million residents are set to join the program.
The pending cuts are just one part of a complex health care picture in California, where experts are far from certain about what the expansion of Medi-Cal will mean for physicians and patients.
"I think we’re going to have a real problem in California with all the new Medi-Cal patients," said Dr. Mark Dressner, who works at a federally qualified health center in Long Beach and is the president of the California Academy of Family Physicians. "Who is going to see them when there’s going to be so many other people in the system?"
The Kaiser Family Foundation estimates that between 990,000 and 1.4 million individuals, mostly single adults, will enter Medi-Cal by 2019 because of the ACA-permitted expansion. Currently, about 8.5 million residents are enrolled. Newly eligible individuals will be enrolled in the program’s managed care health plans.
These new patients could have a hard time finding a doctor. Medi-Cal is one of the lowest payers in the nation, paying between $18 and $24 for an office visit, according to the California Medical Association.
That’s about to be compounded by a pay cut approved by the state and the Centers for Medicare and Medicaid Services in 2011. Physicians tried unsuccessfully to fight the cut in court. Now the state is implementing it retroactively, which means that Medi-Cal payments could be cut 15%-20% over the next few years.
"It really undermines efforts to successfully implement the Affordable Care Act in California," said Lisa Folberg, vice president of medical and regulatory policy at the California Medical Association.
There are broad exceptions to the cut. It does not apply to most primary care services in either managed care plans or fee-for-service Medi-Cal, or to specialty services provided through managed care plans, Ms. Folberg said. And some managed care companies have announced that they will use their discretion in setting payment rates to shield their contracted physicians from the cuts.
"Unfortunately, that doesn’t help the cancer patient on Medi-Cal in Bakersfield who has fee-for-service Medi-Cal and can’t find an oncologist," Ms. Folberg said.
Dr. Darin Latimore, president of the California chapter of the American College of Physicians, said large health systems likely will be able to work around the cuts, using group visits and physician extenders. But small physician practices in rural areas aren’t equipped to make those changes, he said.
"They are not in a position to move work on to others in order to be more efficient and see more Medi-Cal patients," said Dr. Latimore, associate dean of medicine at the University of California Davis.
The result will be that physicians who work outside of the state’s safety net system will be less likely to participate in the Medi-Cal program or will strictly limit the number of patients they see. That will translate to longer waits to get an appointment and shorter visits for Medi-Cal patients.
Another concern: Patients entering Medi-Cal managed care plans might not have access to a broad network of physicians. While California has network adequacy laws, state oversight is inadequate, according to Ms. Folberg. For the most part, the plans are on an honor system.
There are some bright spots for the Medi-Cal expansion. The ACA includes an increase in Medicaid payments to physicians for 146 primary care services provided in 2013 and 2014. The provision temporarily raises payments up to Medicare rates, which for California physicians means a 136% hike on average, according to an analysis from the Kaiser Family Foundation.