DALLAS – Reassurance regarding the cardiovascular benefits of statin therapy in the elderly, even in those above age 75, is provided by a new meta-analysis by the international Cholesterol Treatment Trialists’ Collaboration.
The meta-analysis, which included 174,099 participants in 27 major, published, randomized controlled trials with a median follow-up of 4.9 years, should go a long way toward banishing physician and patient uncertainty about the appropriateness of statin therapy in the elderly. It’s evident that such uncertainty is widespread from recent studies indicating only about half of patients over age 65 are on statin therapy post myocardial infarction (MI). Moreover, the controversial new prevention guidelines don’t address the use of statins in patients over age 75, citing a lack of persuasive evidence because such patients were often excluded from participation in the major statin trials (J. Am. Coll. Cardiol. 2013 [doi: 10.1016/j.jacc.2013.11.002]).
Yet in the new meta-analysis by the University of Oxford–based Cholesterol Treatment Trialist's Collaboration, 7% of all participants – that’s nearly 13,000 patients – were over age 75. That’s a large enough number to be able to draw tentative conclusions. In addition, another 33% of subjects in the meta-analysis were aged 66-75 years, Dr. Jordan Fulcher observed in presenting the results at the American Heart Association scientific sessions.
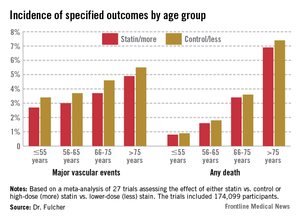
Dividing the nearly 175,000 subjects into four age groups – 55 and younger, 56-65, 66-75, and over 75 – it quickly became apparent to the investigators that while statin therapy significantly reduced nonfatal MI, cardiovascular death, all-cause mortality, and major vascular events in each of the four age groups, there was also a significant trend for smaller relative risk reductions with advancing age.
For example, the incidence of nonfatal MI or coronary heart disease (CHD) death in statin-treated patients aged 55 years or younger was 1.1%, compared with 1.5% in controls, for a 31% relative risk reduction per 39 mg/dL decrease in low-density lipoprotein (LDL) cholesterol, while in the over-75 group the rates were 2.8% versus 3.3%, for a less robust 24% relative risk reduction, reported Dr. Jordan Fulcher of the University of Sydney, Australia.
Looking at major vascular events, which is a broader composite outcome composed of nonfatal MI, CHD death, stroke, or coronary revascularization, patients aged 55 years or less who achieved a 39-mg/dL reduction in LDL had a 25% reduction compared with controls. This relative risk reduction was whittled down to 15% in the over-75s after adjustment for baseline differences in hypertension, gender, diabetes, prior cardiovascular disease, smoking, and creatinine clearance.
Nonetheless – and this is a key study finding – because of the increasing absolute risk of major events with advancing age, the number needed to treat in order to prevent one additional event is "almost identical" across all age groups, according to Dr. Fulcher.
"We therefore conclude that elderly patients at risk should be considered equally as younger patients for statin therapy," he said.
The meta-analysis showed no evidence of favorable or adverse effects of statin therapy on cancer incidence or mortality or on nonvascular mortality in any age group.
Session chair Dr. Lori Mosca said that "as a card-carrying epidemiologist," she thinks it’s important to emphasize for the benefit of nonepidemiologists the truism that relative risk reductions for effective therapies get smaller as people get older because the background rate of disease goes up.
"Relative risk is used for etiology. Absolute risk is used for treatment decisions. I don’t really care if the relative risk [reduction] gets lower as we get older. That has nothing to do with the importance of statins in older patients. It could potentially be more important to treat the elderly despite a lower relative risk" reduction, said Dr. Mosca, professor of medicine at Columbia University, New York, and director of preventive cardiology at New York–Presbyterian Hospital.
The Cholesterol Treatment Trialists’ Collaboration was established back in 1994 in early recognition that no single statin megatrial would have sufficient size and statistical power to answer all the key future clinical issues to arise. The trialists’ database includes virtually all the landmark statin trials whose acronyms are household names within medicine.
Funding for the trialists’ ongoing work is provided by the U.K. Medical Research Council and other national health research organizations. Dr. Fulcher reported having no financial conflicts of interest.