An incentivized, system-based approach to improve care for patients with diabetes and other chronic diseases appeared to pay off after just 3 years by significantly cutting the incidence of adverse clinical events among 25,000 patients with diabetes managed in a single U.S. health care system.
The first 3 years, starting in 2006, of tracking physician performance in applying a nine-item diabetes-management "bundle" to patients in the Geisinger Health System in rural Pennsylvania resulted in improved patient care that prevented about 300 myocardial infarctions, 140 strokes, and 160 cases of retinopathy, according to Dr. Peter B. Berger.
While the results of this adjusted analysis that used a historic control were "fabulous," they were also a little "tough to believe," admitted Dr. Berger, chairman of cardiology at Geisinger in Danville, Pa. Tough to believe because the benefits appeared quickly for endpoints thought to take years or decades to develop, and because of likely confounding by effects not fully controlled by statistical adjustments.
"There is potential for confounding that is impossible to eliminate entirely," he said in an interview.
Nonetheless, the finding is likely real, said Dr. Frederick J. Bloom Jr., a family medicine physician and chief of the care continuum at Geisinger. "We are looking at the impact of improving multiple risk factors including blood pressure, hemoglobin A1c, and low-density lipoprotein [LDL] cholesterol. The literature supports getting some pretty rapid clinical improvements" when all risk factors significantly improve at the same time, Dr. Bloom said in an interview.
Geisinger employs more than 1,000 physicians, runs several hospitals and more than 40 clinics, and provides care to about 2.6 million patients spread through a large area of north-central Pennsylvania. Almost a decade ago Geisinger began to introduce patient management bundles, including bundles for diabetes, hypertension, coronary artery disease, and adult prevention. A high level of compliance with all four of these bundles by all the physicians in a Geisinger office gains for all physicians working in that office a bonus of $10,000 each per year.
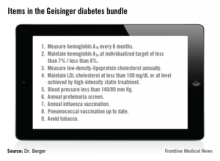
The diabetes bundle contains nine elements (see chart). The hemoglobin A1c, blood pressure, and LDL cholesterol goals have changed over the past 9 years. Currently, the goal for hemoglobin A1c level may be set from less than 7% to less than 8% based on a patient’s age and a shared decision between the patient and physician; the blood pressure goal is less than 140/80 mm Hg; and the LDL cholesterol goal is either less than 100 mg/dL or whatever is achieved with a high-intensity statin regimen.
Geisinger scores its physicians by tallying the percent of patients with diabetes who meet all nine goals of the bundle. Before the program began, in early 2006, this happened for 2.4% of patients. By last August, all the goals had been met by 14.5% of Geisinger patients with diabetes.
"Although 14.5% may seem low, it’s the highest rate in Pennsylvania, and among the highest in the United States. It’s almost uniquely high," Dr. Berger said.
"By using an all-or-none metric, we’re on a different scale; 14.5% is a really good score" for meeting every goal of the diabetes bundle, Dr. Bloom said. Some individual Geisinger sites have had their full compliance rate rise above 20%, showing that more improvement is possible, he added. The biggest challenge is getting patients to meet their blood pressure, hemoglobin A1c, and LDL cholesterol goals.
But the real aim is not good numbers but better clinical outcomes, something that Dr. Berger’s data documented for the first time. The adjusted analysis showed that compared with a propensity score–matched control group drawn from a different health system during the same period, the first 3 years of running the diabetes bundle and offering physician incentives led to one less myocardial infarction for every 82 patients with diabetes managed at Geisinger, one less retinopathy for every 152 patients managed, and one less stroke for every 170 patients managed.
"One difficulty for health systems is to decide how much to invest in these kinds of initiatives and what will be the return on their investment," Dr. Bloom said. "Seeing that these systems of care can produce a quick return will have a profound impact on how people think about investing in these systems," he predicted.
From the provider’s perspective, a financial incentive like the one Geisinger offers "gets people’s attention, but what really sustains the effort is when physicians see patients do better and have better outcomes," he added. While all elements of Geisinger’s approach may not be generalizable to other health care settings, three basic features are: a team-based system of care, data-driven redesign, and incentives, Dr. Bloom said.