CHICAGO– Prepare for sticker shock: Researchers have put a price tag on direct medical expenditures for treatment-resistant hypertension, and it’s a big one.
Indeed, apparent treatment-resistant hypertension (aTRH) is associated with an estimated $11.3-$17.9 billion per year in direct medical expenditures above and beyond expenditures for nonresistant hypertension in the United States, Steven M. Smith, Pharm.D., reported at the American Heart Association scientific sessions.
This is a conservative estimate based on an assumed 5% prevalence of aTRH among U.S. adults with hypertension, which may be a low figure, according to Dr. Smith of the University of Florida, Gainesville.
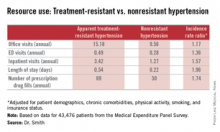
He presented an analysis of data on direct medical expenditures and health care utilization for 43,476 patients with hypertension in the nationally representative U.S. Medical Expenditure Panel Survey, of whom 1,924 met the criteria for aTRH as defined by a requirement for drugs from at least four antihypertensive medications classes in order to achieve blood pressure control.
While aTRH is known to be associated with higher rates of major adverse cardiovascular events and increased mortality relative to nonresistant hypertension, the financial costs associated with this condition haven’t previously been carefully examined.
Mean annual health care expenditures for individuals with aTRH were $20,018, more than twice the $9,814 figure for patients with nonresistant hypertension. But patients with aTRH were older, heavier, less likely to have a high income, and differed in additional ways from the much larger group with nonresistant hypertension. In a multivariate analysis adjusted for these potential confounders, aTRH was associated with $2,413 in excess annual medical expenditures and $1,253 in excess total prescription expenditures, for a total of $3,647 excess total annual health care expenditures per person, compared with subjects with nonresistant hypertension.
New preventive strategies are clearly in order, Dr. Smith concluded.
He reported having no financial conflicts regarding this study, which was conducted without industry funding.