Conference Coverage

Evolocumab halved cardiovascular events in OSLER study
Key clinical point: Evolocumab shows impressive LDL lowering and slashes cardiovascular events.
This meta-analysis contributes important preliminary information as the Food and Drug Administration considers approving PCSK9 inhibitors for hypercholesterolemia, and can be met with cautious enthusiasm. But the findings must be confirmed in long-term trials with prespecified CVD endpoints and close monitoring of adverse events.
The encouraging results regarding mortality and myocardial infarctions in particular warrant caution, because most of the trials were of small or moderate size, had short follow-up periods, and were not specifically designed to detect differences in clinical outcomes or rare adverse events. Longer follow-up under real-world conditions is necessary to better characterize the safety profile of these medications.
Miguel Cainzos-Achirica, M.D., of Johns Hopkins Bloomberg School of Public Health, Baltimore, and four other contributors made these remarks in an editorial accompanying Dr. Navarese’s report (Ann. Intern. Med. 2015 [doi:10.7326/M14-2957]). Their financial disclosures are available at www.acponline.org.
FROM ANNALS OF INTERNAL MEDICINE
Monoclonal antibodies that target PCSK9 – namely evolocumab, alirocumab, and bococizumab – not only profoundly reduce LDL cholesterol and lipoprotein(a) in patients with hypercholesterolemia, but also appear to decrease all-cause mortality and the incidence of myocardial infarction, according to a meta-analysis.
To date, no single study of these agents has been powered to show an effect on mortality or cardiovascular events. But “our large-scale report” – a meta-analysis of 24 phase II and phase III randomized clinical trials comparing the biologics against placebo or ezetimibe – “is the first to show [such] a benefit with these novel agents,” said Dr. Eliano Pio Navarese of the division of cardiology, pulmonology, and vascular medicine, Heinrich Heine University, Dusseldorf, and his associates.
The results must be considered preliminary because this study is a meta-analysis of early-phase trials, not a prospective, randomized phase III trial. But because all the sensitivity analyses and subgroup analyses confirmed the main conclusions of the meta-analysis, it is likely that “the overall benefit is robust and justified,” they noted.
Two pharmaceutical companies have applied to the Food and Drug Administration for approval to use the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors evolocumab (Amgen) and alirocumab (Sanofi Aventis) to treat high cholesterol, and four large trials are underway to assess the anti-PCSK9 monoclonal antibodies’ effects on cardiovascular outcomes. If the findings of this meta-analysis are confirmed and these agents are approved, “it could have a profound effect on public health,” Dr. Navarese and his associates said.
All of the 24 trials included in the meta-analysis were funded by industry, and all were multicenter. They involved 10,159 patients with familial, nonfamilial, mixed, or unspecified hypercholesterolemia. Seventeen of the trials were of less than 6 months’ duration, and four were a year or more in length.
The PCSK9 inhibitors reduced LDL cholesterol by 47%, raised HDL cholesterol by 6%, and decreased lipoprotein(a) levels by 26%, compared with placebo or ezetimibe.
All-cause mortality was 0.31% among patients who took PCSK9-targeting monoclonal antibodies, significantly lower than the 0.53% all-cause mortality among patients who did not (odds ratio, 0.45). However, the “clinical event outcomes should be interpreted with caution because the data were derived from a small number of events.” There were 19 deaths among patients receiving the medications and 21 among those not receiving them, Dr. Navarese and his associates noted (Ann Intern. Med. 2015 [doi:10.7326/M14-2957]).
The difference between the two groups in cardiovascular mortality (0.19% vs. 0.33%) was nonsignificant. Again, the number of cardiovascular deaths was small: 12 among patients receiving the medications and 13 among those not receiving them.
Regarding MI, 10 of the reviewed trials (5,195 patients) reported data for this outcome. MI rates were 0.58% among patients receiving PCSK9 inhibitors and 1.00% among those who were not receiving them, a significant reduction. However, there were 19 MIs in each patient group.
The medications were associated with significantly lower rates of elevated serum creatine kinase (1.96% vs 2.31%). This suggests that anti-PCSK9 monoclonal antibodies may exert a muscle-sparing effect, the investigators said.
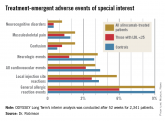
Overall rates of serious adverse events were 9.36% with the medications and 7.73% without them. Rates of treatment discontinuation were similar between the two study groups.
This study was supported in part by CRC 1116 Masterswitches in Myocardial Ischemia, funded by the German Research Council. Dr. Navarese reported having no disclosures; one of his associates reported receiving consulting fees from Sanofi.

Key clinical point: Evolocumab shows impressive LDL lowering and slashes cardiovascular events.
Key clinical point: LDL cholesterol levels below 25 mg/dL induced by a superpotent investigational lipid-lowering agent appear to be safe through...
