What are the possible mechanisms for this patient’s presentation with ischemic stroke?
This patient is presenting with right face and arm weakness with sensory loss, gaze deviation to the left, and expressive aphasia. Abnormalities of speech and gaze paresis that localize to the left frontal lobe with cortical involvement make a subcortical or brainstem lacunar ischemic event less likely. The syndrome is suggestive of a large artery occlusion of the left middle cerebral artery. This type of large artery occlusive disease in the anterior circulation is most often due to an embolus (artery-to-artery or cardiac origin) event and requires arterial imaging of the head and neck acutely as endovascular thrombectomy has been associated with reduced disability compared to intravenous tPA alone.
Further Evaluation
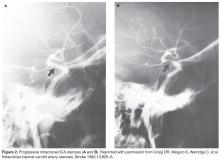
Due to the acute presentation, CT angiography of the head and neck was ordered to assess for a large vessel occlusion. Imaging demonstrated occlusion of a small branch (M3) of the left middle cerebral artery, which was not amenable to endovascular treatment. Additionally, the patient was noted to have severe stenosis of the left supraclinoid (intracranial) internal carotid artery (ICA) with minimal calcified atherosclerotic plaque in the left cervical ICA at the origin without hemodynamically significant stenosis ( Figure 1 and Figure 2 ).What imaging is recommended to identify patients with ICAD?
The Stroke Outcomes and Neuroimaging of Intracranial Atherosclerosis (SONIA) trial sought to evaluate the reliability of noninvasive imaging modalities to identify a 50%–99% stenosis of large proximal cerebral arteries as compared with the gold standard of conventional angiography [3]. Qualifying vessels included the M1 segment of the middle cerebral artery, the carotid siphon, and intracranial vertebral and basilar arteries. Imaging techniques included MRA head without contrast (time of flight) and TCD ultrasound. Both of these imaging modalities demonstrated a high negative predictive value (NPV) for the presence of a 50%–99% intracranial stenosis; however, the positive predictive value (PPV) for TCD and MRA was only 55% and 66%, respectively. Subsequent studies of contrast-enhanced MRA and CTA of the headhave shown high PPV (78%–94%) and NPV (95%–100%) when compared with cerebral angiography for the detection of 70%–99% ICAD [4,5]. Together these data suggest that TCD and MRA of the head without contrast can be used as screening tools to rule out ICAD when normal; however, subsequent contrast-enhanced MRA or CTA is required when abnormalities are identified.
When choosing the best noninvasive imaging modality for any given patient, concomitant medical issues including renal disease, age, presence of a pacemaker, implantable cardiac defibrillator or other metal, and claustrophobia are factors to consider.
What are the potential mechanisms of ischemic stroke in patients with symptomatic ICAD?
Stroke in the symptomatic ICAD group occurs as a result of either (1) thrombus formation at the site of a high-grade stenosis due to an unstable atherosclerotic plaque, (2) low flow through a narrow, stenotic artery (hypoperfusion) or (3) a combination of atheroembolism and hypoperfusion [6]. While a thrombus can occlude the parent vessel at the site of stenosis, more commonly the thrombus migrates distally as an artery-artery embolism to a smaller caliber artery.