From the University of North Carolina Medical Center (Dr. Daniels) and Renovion (Dr. Durham), Chapel Hill, NC.
To Download a PDF of the Full Article:
ABSTRACT
• Objective: To examine common types of medication errors occurring in patients with HIV, with a focus on patient risk, contributing factors, and interventions that can be employed to address the problem of medication errors in this population.
• Methods: Review of the literature.
• Results: The increased complexity and specialization of HIV care, the presence of comorbidities, and the evolving nature of medication management in patients with HIV place these patients at risk for medication errors and adverse drug events. Many studies of hospitalized patients with HIV have reported high rates of medication errors in this population. The consequences of antiretroviral therapy errors can range from minimal harm to life-threatening toxicities and the possibility of resistance and treatment failure. This review discusses the factors contributing to the high rates of error associated with antiretroviral therapy and details strategies to reduce and prevent errors in these patients.
• Conclusion: A comprehensive approach combining multiple interventions can be used to reduce and prevent antiretroviral medication errors in patients with HIV in order to improve the quality of care for this population.
Great progress has been made in the treatment of HIV over the past several decades. With the advancements in treatment options for HIV, considerable reductions in the morbidity and mortality associated with HIV and HIV-related complications have been realized [1,2]. Antiretroviral therapy (ART) has rapidly evolved, offering different mechanisms of action, improved potency, increased tolerability and reduced pill burdens. As a result, HIV infection has transformed from a terminal illness to a manageable chronic disease.
The success of HIV treatment has created a new set of challenges for health care professionals. Patients with successfully treated HIV can expect to live a nearly normal lifespan [3]. With this extended life expectancy, the number of older adults infected with HIV continues to rise, and care for these patients requires a broader and more comprehensive approach. Although HIV-related illnesses such as opportunistic infections have declined, the rate of non–HIV-related comorbidities among patients with HIV has increased [4]. Large cohort studies have shown an association between the risk for HIV-associated non–AIDS-related conditions and CD4 counts [5,6]. HIV-associated non–AIDS-related conditions include cardiovascular disease, kidney disease, liver disease, central nervous system disease, osteoporosis, and non–AIDS-associated malignancies. These conditions occur either more frequently or are more severe in patients with lower CD4 counts or detectable viral loads, but can also arise or persist in virologically suppressed patients with high CD4 counts [4].
The increased complexity and specialization of HIV care, the presence of comorbidities, and the evolving nature of medication management in this population place these patients at risk for experiencing medication errors and adverse drug events. Patients with HIV often receive care by many providers in many different settings. Clinicians caring for patients with HIV must be familiar not only with the treatment of HIV but also with the management and integration of their patients’ primary care needs. In addition, the rates of hospitalization for HIV-infected patients have declined substantially since the mid-1990s [7]. Of the patients with HIV requiring hospitalization, the proportion of hospitalizations due to opportunistic infections has decreased and the proportion of hospitalizations due to other conditions has increased [7]. For many of these patients, the treatment of HIV has retreated to the background as a stable condition, while the management of other acute illness requires more attention.
An estimated 1.5 million adverse drug events occur each year in the United States due to medication errors [8]. Medication errors are common and can occur at any point during the medication use process, including procurement, prescribing, transcribing, preparing or compounding, dispensing, administration, and monitoring. Any time a patient moves from one setting of health care to another, the risk for medication errors is increased. Several reports have highlighted the increased risk for medication errors and adverse effects that can occur during these transitions of care. In fact, up to 70% of patients have an unintentional medication discrepancy at hospital discharge [9]. Errors during hospital admission are common as well, affecting up to two-thirds of patients admitted to hospitals [10,11].
As HIV care becomes more complex, concerns have been raised regarding increases in the number of medication errors in these patients, especially during transitions of care. Most studies of hospitalized patients with HIV have reported error rates of 5% to 30% [12–15]. One study demonstrated that the risk for a medication error at admission for patients with HIV was 3.8 errors per patient, whereas for patients without HIV the rate was 2.8 errors per patient [16]. Because of the potential for the emergence of resistance mutations, adherence to ART is essential for successful treatment and sustained viral suppression. Thus, medication errors of omission could have particularly detrimental effects for the long-term treatment of patients with HIV. Furthermore, as this population ages, polypharmacy becomes common, placing these patients at risk for errors related to dosing and drug interactions [17]. Because medication errors can lead to patient harm and death as well as increased health care costs, elucidating the reasons for errors associated with HIV management and exploring strategies aimed at the reduction and prevention of errors is essential.
The goal of this review is to examine the common types of medication errors occurring in patients with HIV, with a focus on patient risk, contributing factors, and interventions that can be employed to address the problem of medication errors in this population.
Incidence of ART Errors
Several studies have indicated that the incidence of ART errors in hospitalized patients is rising. The rate of ART errors detected at admission among hospitalized patients increased from 2% in 1996 to 12% in 1998 according to one study [13]. Studies conducted from 2004 to 2007 report ART error rates at hospital admission ranging from 17% to 26% [12,15,18]. In more recent studies, high ART error rates ranging from 35% to 55% have been reported [19–23]. Two studies have reported ART error rates occurring at hospital admission to be as high as 70% [24,25].
Various types of ART medication errors can occur. Commonly reported errors include those related to drug interactions, incorrect dosing, incorrect scheduling, and incomplete regimens. Errors occurring at the time of hospital admission appear to be more common than errors occurring at other time points [20,24,26]. A comprehensive systematic review of studies regarding medication errors in hospitalized patients with HIV found that errors at the point of prescribing encompass the majority of errors [27]. One study identified 82 ART errors occurring at admission in 68 hospitalized patients. Of these errors, 37% occurred at the point of prescribing, 27% were attributed to dispensing, and 18% were attributed to inaccuracies in outpatient clinic documentation [24].
Several authors have drawn associations between the rate of errors and the class of antiretroviral prescribed. Protease inhibitors have been the most frequently implicated drug class [13,18,20,27,28]. In an analysis of 145 ART errors in one hospital, 70% of dosing errors involved protease inhibitors and 30% involved nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs). In addition, scheduling errors occurred most often with protease inhibitors, and errors due to drug interactions were also most likely to involve protease inhibitors [28]. Conversely, another study did not find an association between protease inhibitors and the risk for error compared to other classes of drugs. In fact, this study showed that the NRTI class was associated with an increased risk of prescribing error compared to protease inhibitors and that the use of co-formulated drugs that were available on the hospital formulary protected against error [20]. These findings highlight the various factors contributing to error among different institutions, especially related to hospital formulary selections and availability of specific drugs.
Fewer studies have evaluated ART errors in outpatient settings. One report evaluated the NRTI medication records from an outpatient electronic medical record system from August 2004 to September 2005. A total of 902 NRTI records for 603 patients were analyzed. The overall error rate was 6% (53/902), with renal dosing errors being most common (75% of errors) [29]. Another evaluation of ART errors among privately insured patients with HIV found that the probability of a patient with HIV receiving an inappropriate drug combination in a given year was higher in 2005 (5.9%) compared to 1999 and 2000 (1.9%). Many of the increased errors seen in 2005 compared to 1999–2000 in this study were attributed to errors related to protease inhibitor boosting [30].
Harms and Consequences of ART Errors
The consequences of ART errors can range from minimal harm to life-threatening toxicities and the possibility of resistance and treatment failure. Potential consequences of ART errors are listed in Table 1.Because of the potential for the emergence of drug resistance, adherence to an ART regimen is essential for successful treatment and sustained viral suppression. ART medication errors causing disrupted therapy, omitted drugs, or suboptimal dosing can lead to the development of viral resistance mutations and ultimately treatment failure placing patients at risk for HIV-related complications such as opportunistic infections as well as non–HIV-related complications [31]. Health care providers should recognize the importance of appropriate uninterrupted therapy for this population and should assist in facilitating this effort. On a community level, patients with elevated plasma HIV RNA levels due to untreated disease or treatment failure have a greater risk of transmitting HIV to others [32]. Effective ART on a population basis will have important public health advantages.
In addition to the potential consequences of ART error relating to treatment failure and resistance, ART errors may also lead to drug toxicities and drug intolerance, increasing the risk of nonadherence, and further exacerbating the aforementioned consequences.
ART errors also carry the same consequences as errors involving other non-ART medications, such as loss of patient trust, civil and criminal legal consequences, professional board discipline, and increased health care costs [33]. One study reported a cost avoidance of $24,000 annually for inpatient and $124,000 annually for outpatient through the use of pharmacists’ interventions to prevent errors [34]. Another study found that patients experiencing an ART error related to protease inhibitor boosting incurred claims costing 21.5% more than patients not experiencing a boosting error [30].
Contributing Factors
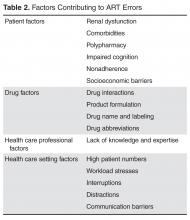
In order to develop effective interventions to minimize and prevent ART errors, it is important to identify contributing factors and seek to understand the cause of errors. Contributing factors may be broadly classified into 1 of 4 categories: patient factors, health care professional factors, medication factors, and factors related to the health care setting (Table 2). A decline in patients’ renal or hepatic function is associated with a higher risk for medication errors [35]. This is of particular importance for NRTI-containing ART regimens because most of the medications in this class require dose adjustment in renal dysfunction. Indeed, an increased risk for dosing errors has been observed among patients with renal dysfunction receiving NRTI drugs [29]. Other patient factors that contribute to the risk for medication errors include impaired cognition, nonadherence, and socioeconomic challenges, all of which are commonly encountered in HIV care. Chronically ill patients and older patients are also at risk for experiencing medication errors. This is likely due to the increased comorbidities, polypharmacy, and longer durations of therapy seen in this population [36]. Patients with HIV are particularly at risk because they require lifelong treatment with multiple drugs. In addition, these patients often require treatment for multiple comorbidities such as cardiovascular disease and diabetes, which further increases their risk.Health care professional–associated factors can also contribute to ART errors. The increasing complexity and specialization of HIV care and the rapidly evolving nature of medication management in this population have created an environment in which many providers without extensive experience in the treatment of HIV are responsible for managing HIV in settings beyond the HIV clinic. A survey of non-HIV specialized physicians conducted in 2007 revealed a poor knowledge base of common ART regimens among these physicians [37]. Likewise, HIV providers may be uncomfortable serving a primary care role for patients with HIV due to their own lack of experience and knowledge of primary care [38]. This issue is becoming more relevant, as non-AIDS comorbidities are emerging as the main health concerns for patients with HIV [39]. Health care professionals’ knowledge of HIV care also contributes to ART errors at other points in the medication use process beyond prescribing. Pharmacists lacking experience in identifying appropriate ART regimens may not recognize errors, and, therefore, may not be able to intervene and prevent errors from occurring.
Medication factors contributing to the risk for errors include risks related to the pharmacologic properties of certain drugs as well as drug naming and labeling factors. Certain antiretroviral classes are known to interact with many medications due to inhibition or induction of metabolic pathways responsible for drug metabolism, such as the cytochrome P-450 pathways. In addition, many antiretroviral medications require “boosting” with another drug to increase systemic exposure of the antiretroviral. Boosting is required for most protease inhibitors and for the integrase inhibitor elvitegravir. For some of these medications, the boosting agent is provided in a co-formulated product. However, for others, a separate prescription for the boosting medication is required. These factors contribute to the risks for drug interactions as well as drug and dosing errors.
Errors may also occur due to drug naming and labeling factors. Confusion due to look-alike/sound-alike medications is common, especially with handwritten or verbally transcribed orders. Examples of look-alike/sound-alike medications include lamivudine/lamotrigine, Viramune/Viread/Viracept, and ritonavir/Retrovir. The use of abbreviations can also lead to error. Reports have described errors associated with zidovudine, which is often abbreviated AZT, being confused with azathioprine [40,41]. An evaluation of ART errors reported to a national medication error reporting program found that look-alike/sound-alike medication names contributed to 19% (77/400) of the errors reported during the 48-month time period evaluated [15].
Several antiretroviral medications are co-formulated into single tablets to decrease pill burden and increase adherence. The use of co-formulated products has the potential to either increase or decrease the risk of errors. Prescribing one co-formulated product rather than its individual components simplifies the prescribing process, allowing the prescriber to become familiar with one product and one dosing scheme in place of 2 or more drugs with different dosing recommendations. The risk of inadvertent omission of a drug and the risk of improper dosing is reduced with the use of co-formulated products. On the other hand, when patients are transitioned from one health care setting to another (such as admission to a hospital), these products may require conversion to the individual components of the drug due to formulary availability and/or cost concerns. Studies have shown that formulary conversions from co-formulated products to individual components are frequently associated with ART errors and that the use of co-formulated products in the inpatient setting reduces these errors [20,22,24,26].
Finally, factors related to the health care setting can influence the risk for errors. High patient numbers, time constraints, and workload stresses can all increase the likelihood that an error will occur [36]. Interruptions and distractions occurring at any point in the medication use process can lead to error.
Transitioning from one health care setting to another also places patients at risk for being harmed by medication errors. Up to 70% of patients may have an unintentional medication discrepancy at hospital discharge, and errors occurring at hospital admission have been reported to affect two-thirds of admitted patients [42]. Many of these errors hold the potential to cause harm to the patient, especially if the errors are carried forward throughout the patient’s admission and after discharge. One study found that 22% of ART errors occurring at hospital admission were attributable to outpatient clinic documentation errors [24]. This highlights the need for improved documentation processes and draws attention to the element of communication at transitional points of care. Lack of adequate resources for medication reconciliation is a widely recognized challenge. This includes resources of personnel as well as electronic medical record systems that can facilitate the reconciliation process. The importance of accurately documenting a patient’s medication history and the ability to easily communicate this information to other health care settings cannot be underestimated. Electronic medical record systems should be developed to facilitate and enhance the processes of reconciliation, documentation, and communication.
Interventions to Address ART Errors
The causes of ART errors are multifactorial and should be addressed using comprehensive approaches tailored to the specific health care setting. Several types of interventions aimed at reducing and preventing ART errors have been evaluated in the literature [12,18,26,27]. In general, these interventions have focused on provider education, use of technology and clinical decision support systems, pharmacist-led medication review and intervention, and hospital formulary changes. Other interventions that may lead to a reduction in ART errors include minimizing polypharmacy, improving medication reconciliation processes during transitions of care, and multidisciplinary follow-up clinic visits after hospital discharge.
Because the sources of ART errors are multifactorial, the optimal strategy to prevent and reduce errors is likely to be a comprehensive approach combining several of the aforementioned interventions. One study showed that a combined approach that included updates to the institution’s computerized physician order entry (CPOE) system, education for the pharmacy and ID departments, and daily review of patients’ medications by pharmacists was successful in reducing the percentage of admissions with an ART error from 50% to 34%. In addition, the time to error resolution decreased from 180 hours to 23 hours, and the error resolution rate increased from 32% to 68% [21]. Another study demonstrated benefits using a comprehensive approach including the dissemination of educational pocket cards for physicians, pharmacists and nurses; CPOE alerts; hospital formulary updates to include co-formulated products; and a daily review of medications by an ID-specialized pharmacist for patients receiving ART. These strategies resulted in a reduced ART error rate from 72% to 15% in 7 months [26]. These studies demonstrate the benefit of multifaceted strategies to reduce ART error rates.
Education
Given the complexity of HIV care and overall lack of antiretroviral medication knowledge among non-ID specialized health care professionals, educational programs aimed at increasing the comfort level and familiarity of ART is important [16,37]. Frequent training to update health care professionals on the newest recommendations for HIV management can help achieve this goal [19,27]. Educational interventions aimed at reducing medication errors have been shown to be transiently effective but may lack sustained effects [43]. Educational programs for health care professionals should be designed to provide frequent brief updates, and are likely to be more successful when combined with other approaches [19,26].
Education directed toward patients, families, and caregivers can also play a pivotal role in error prevention. Patients should be encouraged to use one pharmacy, if possible, to ensure that one complete, accurate, and current profile is maintained. The use of one pharmacy can also assist in the identification of therapeutic duplications and drug interactions. Counseling patients with visual aids, such as charts with pictures of drugs, can also be used as a tool for education. Patients who are familiar with the names and the appearances of their drugs are more likely to recognize errors. In addition, patients should be advised to maintain their own current medication list so that they will be able to provide this information to all of the health care professionals involved in their care [33,44].
Technology and Clinical Decision Support Systems
Overall, the increasing use of technology such as CPOE, decision support systems, and barcoding systems has been shown to decrease the risk of medication error [19,45,46]. Guo et al observed a 35% decrease in ART error rates after the integration of customized order entry sets into an existing CPOE program [19]. Another study reported a 50% decrease in the ART error rate after the introduction of an electronic medical record system [45]. On the other hand, some reports evaluating the role of CPOE systems to reduce medication error rates are conflicting [15,19,23,48]. Differences in system capabilities and programming and differing needs and challenges of institutions may account for the varying results reported in the literature. CPOE systems can serve as valuable tools for assisting in medication prescribing. Confusion due to abbreviations, illegible writing and look-alike/sound-alike drugs should be eliminated or greatly reduced with the use of CPOE. However, the limitations of these systems, which may differ among different systems, should be appreciated. As ART regimens and dosing recommendations change, clinical decision support systems can quickly become out-of-date and require frequent updating. One study identified fields that pre-populated drug names and frequencies within a CPOE system to be the cause of several medication errors [16]. Studies have also identified errors related to disregarded alerts from decision support software [15,16]. “Alert fatigue” is a well-recognized phenomenon that occurs when clinicians are exposed to a large volume of clinical decision support alerts of varying clinical significance. Over time, clinicians begin to become desensitized to the alerts, and they may eventually stop responding to them.
Some limitations of CPOE systems arise from the individual system capabilities. Some systems have the ability to check for appropriate dosing, recommend adjustments in renal dysfunction, and provide alerts for drug interactions, but some systems lack these capabilities. In addition, CPOE systems are often not able to prevent errors of omission, delays in continuation of therapy, and medication scheduling errors [15,45].
Given the limitations of CPOE and clinical decision support technologies, it is unlikely that these interventions alone will be sufficient to fully address the problem of ART errors. These technologies can, however, serve as a powerful tool in the prevention and reduction of ART errors, especially when used in combination with other strategies.
Pharmacist Intervention
Multiple studies have shown that clinical pharmacists are effective at decreasing ART medication errors in the inpatient setting [12,18,23,25,28,45,49,50]. One institution implemented an HIV-specialized pharmacist review strategy that decreased the median time to error correction from 84 hours to 15.5 hours among hospitalized patients [12]. Corrigan et al showed that a review of medications by an HIV-specialized pharmacist 48 hours after hospital admission decreased error rates from 52% to 5% [50]. Another study showed that with the use of an electronic medical record, errors among hospitalized patients with HIV were 9.4 times more likely to be corrected within 24 hours when an HIV-specialized pharmacist was consulted [45].
The majority of studies evaluating the effect of pharmacist interventions have utilized the services of a pharmacist with specialized training in HIV. Few studies have evaluated the impact of interventions by pharmacists without this specialized training. One study retrospectively evaluated and characterized ART errors among hospitalized patients. Medication reconciliation was performed within 24 hours of admission by unit-based pharmacists without specialized training in HIV. Overall, 30.8% of errors were corrected within 24 hours and 14.2% were corrected after 24 hours. However, 54.7% of the errors were not recognized and were never corrected [20]. Just as physicians trained in general medicine lack knowledge of antiretroviral medications, pharmacists without HIV-specialized training may also be less familiar with current ART recommendations [16,37].
Overall, the studies evaluating the impact of pharmacist intervention on reducing ART error rates have shown significant reductions in time to error corrections. The nature of this type of intervention however, lends itself to correction of errors rather than prevention of errors. Indeed, one hospital reported an ART error rate of 29% on the first day of admission compared to 7% on the second day of admission, a decrease that was attributed to retrospective review of medication orders by clinical pharmacists. This study also noted the occurrences of additional errors identified on the second day of admission, highlighting the importance of daily review and follow-up throughout the hospital stay [28].
Hospital Formulary Selections
Several studies have documented an association between hospital formulary options and ART errors [20,22,24,26]. The prescribing of ART medications that are not available on hospital formulary is consistently associated with higher rates of error. Many hospitals minimize the numbers of different medications offered through the maintenance of a formulary. Formularies assist in reducing costs, preserving storage space, and simplifying prescribing. Because some hospitals choose to exclude co-formulated products from the formulary, several ART medications may not be included. In addition, some ART medications may be excluded from formulary due to their infrequent use or higher costs. The extra step of converting a co-formulated product to its individual components increases the risk for errors. In one study, the addition of all co-formulated ART medications to the hospital formulary in combination with several other interventions had a significant effect on reducing the ART error rate [26].
Transitions of Care Interventions
Patients with HIV are at risk for experiencing medication errors and discrepancies any time they transition from one health care setting to another. Hospitalization poses the highest risk as it often disrupts continuity of care and corresponds with a comparatively larger number of medication changes [16,51]. This risk is present on admission, throughout hospitalization, and upon discharge. Perhaps the errors of greatest concern are those that are carried forward after discharge on to the outpatient setting. Medication discrepancies at transitions of care have been associated with increases in adverse events and increased hospital readmission rates [52,53]. One study evaluating adverse events in geriatric patients transitioning from hospital to home found that the most frequently reported adverse events after discharge were related to incorrect drugs or dosages of medication regimens [54]. Tools that can assist in integration and coordination during transitions of care are greatly needed.
One of the most important strategies to prevent and correct medication discrepancies during transitions of care is medication reconciliation. Several studies have demonstrated the efficacy of medication reconciliation in decreasing medication errors [55]. Medication reconciliation is especially important for patients taking many medications. An estimated 14% of patients with HIV older than age 65 take 4 or more medications [56]. This population often requires treatment for other chronic conditions such as hypertension, diabetes, and depression, further increasing the risk for adverse drug events including medication error. Because of the complexities associated with the treatment of HIV and the increased risk for errors, routine medication reconciliation among this population should be a priority.
In addition to medication reconciliation, several studies have evaluated the effects of coordinated pharmacist or multidisciplinary post-discharge follow-up visits for medication therapy management as a strategy to reduce preventable medication-related adverse events [57–59]. Patients receiving clinic-based medication therapy management by a clinical pharmacist after hospital discharge had a lower 60-day hospital readmission rate compared to those who did not have a clinic visit with a pharmacist (18.2% vs. 43.1%) [59]. Another study compared 2 models of post-discharge follow-up, a multidisciplinary team model led by a clinical pharmacist compared to a standard physician-only model. The goal of the multi-disciplinary team model was to complete a thorough medication review, address lifestyle interventions, and address barriers to care. Overall, patients seen by the multidisciplinary team had a 30-day hospital readmission rate of 14.3% compared with a 34.3% readmission rate in the physician-only team [58]. Many different care models have been proposed to improve continuity of care for patients with HIV. The ideal model is not known, and it is likely that several different models would be effective. Optimal models should integrate the patient-physician relationship with multidisciplinary team approaches [60].
Conclusion
The rapidly evolving nature of HIV management and the increase in non–HIV-related comorbidities among this population has created a landscape that places these patients at risk for medication errors. Although ART has improved survival, medication errors place these patients at risk for adverse events and treatment failure. Medication errors are particularly likely to occur during transitions of care. Several interventions to prevent and decrease ART errors have been evaluated including educational strategies, hospital formulary changes, use of technology, and medication review and intervention by clinical pharmacists. However more research is needed to determine optimal strategies to address ART medication errors. Successful approaches have implemented comprehensive methods combining multiple interventions aimed at addressing several distinct sources of error. Promotion of a culture of safety is also an important component of medication error management. Health care professionals should be encouraged to report errors, and lessons learned from errors should be used to guide efforts to prevent future errors. Finally, improved integration of care with a focus on systematic initiatives for medication reconciliation as well as multidisciplinary approaches to transitions of care will be essential for reducing the rate of medication error among patients with HIV.
Corresponding author: Lindsay M. Daniels, PharmD, Lindsay.Daniels@unchealth.unc.edu.
Financial disclosures: None.
References
1. Egger M, May M, Chene G, et al. Prognosis of HIV-1 infected patients starting highly active, antiretroviral therapy: a collaborative analysis of prospective studies. Lancet 2002;360:119–29.
2. Palella FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998;338:853–60.
3. May MT, Gompels M, Delpech V, et al. Impact on life expectancy of HIV-1 positive individuals of CD4 cell count and viral load response to antiretroviral therapy. AIDS 2014; 28:1193–202.
4. Greene M, Justice AC, Lampiris HW, Valcour V. Management of HIV infection in advanced age. JAMA 2013;309:1397–1405.
5. Baker JV, Peng G, Rapkin J, et al. CD4+ count and risk of non-AIDS diseases following initial treatment of HIV infection. AIDS 2008;22:841–8.
6. Monforte A, Abrams D, Pradier C, et al. HIV-induced immunodeficiency and mortality from AIDS-defining and non-AIDS-defining malignancies. AIDS 2008;22:2143–53.
7. Buchacz K, Baker RK, Moorman AC, et al. Rates of hospitalizations and associated diagnoses in a large multisite cohort of HIV patients in the United States, 1994-2005. AIDS 2008;22:1345–54.
8. Aspden P, Wolcott J, Bootman JL, et al. Preventing medication errors: quality chasm series. Washington DC: National Academies Press; 2007.
9. Kripalani S, Roumie CL, Dalal AK, et al. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Ann Intern Med 2012;157:1–10.
10. Tam VC, Knowles SR, Cornish PL, et al. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ 2005;173:510–515.
11. Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chonic diseases. JAMA 2011;306:840–7.
12. Heelon M, Skiest D, Tereso G, et al. Effect of a clinical pharmacist’s interventions on duration of antiretroviral-related errors in hospitalized patients. Am J Health Syst Pharm 2007;64:2064–8.
13. Purdy BD, Raymond AM, Lesar TS. Antiretroviral prescribing errors in hospitalized patients. Ann Pharmacother 2000;34:833–8.
14. Gray J, Hicks RW, Hutchings C. Antiretroviral medication errors in a national medication error database. AIDS Patient Care STDS 2005;19:803–12.
15. Rastegar DA, Knight AM, Monolakis JS. Antiretroviral medication errors among patients with HIV infection. Clin Infect Dis 2006;43:933–8.
16. Snyder AM, Klinker K, Orrick JJ, et al. An in-depth analysis of medication errors in hospitalized patients with HIV. Ann Pharmacother 2011;45:459–68.
17. Edelman EJ, Gordon KS, Glover J, et al. The next therapeutic challenge in HIV: polypharmacy. Drugs Aging 2013;30:613–28.
18. Carcelero E, Tuset M, Martin M, et al. Evaluation of antiretroviral-related errors and interventions by the clinical pharmacist in hospitalized HIV-infected patients. HIV Medicine 2011;12:494–9.
19. Guo Y, Chung P, Weiss C, et al. Customized order-entry sets can prevent antiretroviral prescribing errors: a novel opportunity for antimicrobial stewardship. P T 2015;40:353–8.
20. Commers T, Swindells S, Sayles H, et al. Antiretroviral medication prescribing errors are common with hospitalization of HIV-infected patients. J Antimicrob Chemother 2014;69:262–7.
21. Sanders J, Pallotta A, Bauer S, et al. Antimicrobial stewardship program to reduce antiretroviral medication errors in hospitalized patients with HIV infection. Infect Control Hosp Epidemiol 2014;35:272–7.
22. Chiampas TD, Kim H, Badowski M. Evaluation of the occurrence and type of antiretroviral and opportunistic infection medication errors within the inpatient setting. Pharm Pract 2015;13:512.
23. Eginger KH, Yarborough LL, Inge LD, et al. Medication errors in HIV-infected hospitalized patients: a pharmacist’s impact. Ann Pharmacother 2013;47:953–60.
24. Pastakia SD, Corbett AH, Raasch RH, et al. Frequency of HIV-related medication errors and associated risk factors in hospitalized patients. Ann Pharmacother 2008;42:491–7.
25. Garey KW, Teichner P. Pharmacist intervention program for hospitalized patients with HIV infection. Am J Health Syst Pharm 2000;57:2283–4.
26. Daniels LM, Raasch RH, Corbett AH. Implementation of targeted interventions to decrease antiretroviral-related errors in hospitalized patients. Am J Health Syst Pharm 2012;69:422–30.
27. Li EH, Foisy MM. Antiretroviral and medication errors in hospitalized HIV-positive patients. Ann Pharmacother 2014;48:998–1010.
28. Yehia BR, Mehta JM, Ciuffetelli D, et al. Antiretroviral medication errors remain high but are quickly corrected among hospitalized HIV-infected adults. Clin Infect Dis 2012;55:593–99.
29. Willig JH, Westfall AO, Allison J, et al. Nucleoside reverse-transcriptase inhibitor dosing errors in an outpatient HIV clinic in the electronic medical record era. Clin Infect Dis 2007;45:658–61.
30. Hellinger FJ, Encinosa WE. The cost and incidence of prescribing errors among privately insured HIV patients. Pharmacoeconomics 2010;28:23–34.
31. Deeks SG, Gange SJ, Kitahata MM, et al. Trends in multidrug treatment failure and subsequent mortality among antiretroviral therapy-experienced patients with HIV infection in North America. Clin Infect Dis 2009;49:1582–90.
32. Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011;365:493–505.
33. Wittich CM, Burkle CM, Lanier WL. Medication errors: an overview for clinicians. Mayo Clin Proc 2014;89:1116–25.
34. Merchen BA, Gerzenshtein L, Scarsi KK, et al. Evaluation of HIV-specialized pharmacists’ impact on prescribing errors in hospitalized patients on antiretroviral therapy. 51st Interscience Conference on Antimicrobial Agents and Chemotherapy; 2011 Sep 17-20; Chicago IL. Abstract H2–794.
35. Lesar TS, Briceland L, Stein DS. Factors related to errors in medication prescribing. JAMA 1997;277:312–17.
36. Agu KA, Oqua D, Adeyanju Z, et al. The incidence and types of medication errors in patients receiving antiretroviral therapy in resource constrained settings. PLoS ONE 2014;9:e87338.
37. Arshad S, Rothberg M, Rastegar DA, et al. Survey of physician knowledge regarding antiretroviral medications in hospitalized HIV-infected patients. J Int AIDS Soc 2009;12:1.
38. Fultz SL, Goulet JL, Weissman S, et al. Differences between infectious diseases-certified physicians and general medicine-certified physicians in the level of comfort with providing primary care to patients. Clin Infect Dis 2005;41:738–43.
39. Cheng QJ, Engelage EM, Grogan TR, et al. Who provides primary care? An assessment of HIV patient and provider practices and preferences. J AIDS Clin Res 2014;5:366.
40. Cohen MR, Davis NM. AZT is a dangerous abbreviation. Am Pharm 1992;32:26.
41. Ambrosini MT, Mandler HD, Wood CA. AZT: zidovudine or azathioprine? Lancet 1992;339:935.
42. Sponsler KC, Neal EB, Kripalani S. Improving medication safety during hospital-based transitions of care. Cleve Clin J Med 2015;82:351–60.
43. Peeters MJ, Pinto SL. Assessing the impact of an educational program on decreasing prescribing errors at a university hospital. J Hosp Med 2009;4:97–101.
44. Faragon JJ, Lesar TS. Update on prescribing errors with HAART. AIDS Read 2003;13:268–78.
45. Batra R, Wolbach-Lowes J, Swindells S, et al. Impact of an electronic medical record on the incidence of antiretroviral prescription errors and HIV pharmacist reconciliation on error correction among hospitalized HIV-infected patients. Antivir Ther 2015:2040–58.
46. Keers RN, Williams SD, Cooke J, et al. Impact of interventions designed to reduce medication administration errors in hospitals: a systematic review. Drug Saf 2014;37:317–32.
47. Reckmann MH, Westbrook JI, Koh Y, et al. Does computerized provider order entry reduce prescribing errors for hospital inpatients? A systematic review. J Am Med Inform Assoc 2009;16:613–23.
48. Bozek PS, Perdue BE, Bar-Din M, Weidle PJ. Effect of pharmacist interventions on medication use and cost in hospitalized patients with or without HIV infection. Am J Health Syst Pharm 1998;55:1151–5.
49. De Maat MM, de Boer A, Koks CH, et al. Evaluation of clinical pharmacist interventions on drug interactions in outpatient pharmaceutical HIV care. J Clin Pharm Ther 2004;29:121–30.
50. Corrigan MA, Atkinson KM, Sha BE, Crank CW. Evaluation of pharmacy-implemented medication reconciliation directed at antiretroviral therapy in hospitalized HIV/AIDS patients. Ann Pharmacother 2010;44:222–3.
51. Rao N, Patel V, Grigoriu A, et al. Antiretroviral therapy prescribing in hospitalized HIV clinic patients. HIV Med 2012;13:367–71.
52. Coleman EA, Smith JD, Raha D, Min S. Posthospital medication discrepancies. Arch Intern Med 2005;165:1842–7.
53. Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med 2003;138:161–7.
54. Mesteig M, Helbostad JL, Sletvold O, et al. Unwanted incidents during transition of geriatric patients from hospital to home: a prospective observational study. BMC Health Serv Res 2010;10:1.
55. Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med 2012;172:1057–69.
56. Hasse B, Ledergerber B, Furrer H, et al. Morbidity and aging in HIV-infected persons: the Swiss HIV Cohort Study. Clin Infect Dis 2011;53:1130–9.
57. Downes JM, O’Neal KS, Miller MJ, et al. Identifying opportunities to improve medication management in transitions of care. Am J Health Syst Pharm 2015;72:S58–69.
58. Cavanaugh JJ, Lindsey KN, Shilliday BB, Ratner SP. Pharmacist-coordinated multidisciplinary hospital follow-up visits improve patient outcomes. J Manag Care Spec Pharm 2015;21:256–60.
59. Bellone JM, Barner JC, Lopez DA. Postdischarge interventions by pharmacists and impact on hospital readmission rates. J Am Pharm Assoc 2012;52:358–62.
60. Handford CD, Tynan AM, Rackal JM, Glazier RH. Setting and organization of care for persons living with HIV/AIDS. Cochrane Database Syst Rev 2006;19:CD004348.