Screenings were offered in the public housing units 3 times a week (twice during the week and once during the weekend). Posters in the neighborhood notifed women of the time and location of the screenings. Other settings for services such as screenings and referrals to primary care and health insurance applications included churches, mosques, community festivals, farmers markets, parks, and hair salons.
Women who had elevated glucose readings were invited to enroll in the DCCP program and an appointment at the WSHC was made for those who signed up.
During the period January 2012 to June 2013, 980 African-American women were screened for diabetes. Most screenings took place in the public housing units. Among those screened, 340 had an elevated blood glucose and were referred to WSHC for services. Of those, 175 women were recruited and enrolled into the DCCP. At the WSHC, a standardized protocol was used to measure HbA1c to confirm a diagnosis of diabetes once patients attended their first appointment. Age of participants ranged from 40 to 49. Most women were unemployed and had many competing responsibilities and stressors. Completed preassessment questionaires indicated that participants did not engage in healthy eating or physical activity as part of their daily routines prior to enrollment.
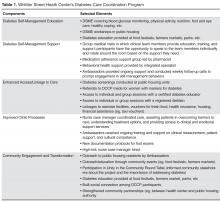
Program Components
Core components of the DCCP included 1) diabetes self-management education, 2) support for managing diabetes and distress, 3) enhancing access and linkage to care, 4) improving quality of care, 5) community organization, mobilization, and advocacy, and 6) health system and community transformation ( Table 1 ).At the Center, Ambassadors spoke with program participants and inquired about their barriers to diabetes care (eg, access to food [15], health insurance, etc.) using a standardized list. Ambassadors linked program participants to community support services as needed, including health insurance enrollment, financial support, and housing support. Services were also provided in collaboration with community organizations. For example, subsidized gym memberships were available at the local YMCA and a local fitness studio, and there was an instructor at the YMCA to guide the women through physical activity routines.
Participants could attend DSME group sessions provided by the certified diabetes educator. The course met twice a week for 2 hours for a period of 6 weeks. The course was interactive and included hands-on training in blood glucose measurement and food preparation. Healthy food was offered after each session, which provided a further opportunity for participants to engage in peer-to-peer support. After the completion of the DSME course, bi-weekly support group sessions were held until program completion (June 2013). All clinical team members were present at the support group sessions, with patients rotating to speak to them to ask questions or discuss concerns related to self-management.
A part of DSME, the registered dietitian provided nutrition information and healthy cooking demonstrations for program participants within group sessions. The primary care physician met the patient once a month and kept track of clinical changes over time. Patients with HbA1c ≥ 9% were referred to the high-risk nurse case manager who worked one-on-one with program participants to help them avoid serious diabetes complications.