Items within each domain have equal value (ie, each question on the checklist is worth 1 point) and the sum of points yields the quantifiable assessment of how well patients are performing in each area of their health. Assessment meetings occur monthly when eligible patients are discussed. Domains are evaluated by the health care provider responsible for his/her own domain (eg, social worker completes the psychosocial domain, the academic coordinator completes the academic domain, etc.).
PDSA Methodology
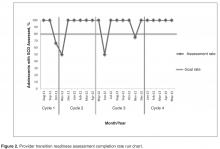
PDSA (Plan-Do-Study-Act) methodology was utilized to develop and evaluate the assessment tool. PDSA is a QI method that utilizes small-scale changes to a process, primarily within health care environments [16]. PDSA is executed in cycles and as changes are made, the process acted upon is improved. Changes are tested on a small scale and barriers are identified. Adjustments are made in subsequent cycles and as needed. For the QI project, 3 PDSA cycles were completed for the development and implementation of the assessment tool ( Figure 1 ). We established a goal of completing an assessment for 80% of eligible patients ( Figure 2 ). We used the clinical database to track this goal for each PDSA cycle. The period of data collection was August 2011 through May 2013. All adolescents receiving medical care in the SCD teen clinic aged 17 and 18 years were eligible for evaluation. From August 2011 to June 2013 we assessed 72 patients (53% male), median age 17.04 years. The following sickle cell genotypes were represented: 40 HbSS, 19 HbSC, 8 HbSβ +, 3 HbSβ 0, and 2 HbS/HPFH. The data were collected for this report with institutional review board approval.Cycle 1
The objective of the first cycle was to assess feasibility and acceptability of the assessment tool. Patients were assessed during the month of their 17th birthday. Fourteen out of 16 eligible patients (87.5%) were assessed: 1 patient was lost to follow-up, and 1 patient inadvertently was not included in the assessment due to an administrative error. Feedback from the first cycle revealed that some items on the emotional/cognitive domain checklist were not clearly defined, and there was some overlap with the psychosocial domain checklist. Additionally, some items were not readily assessed by psychology based on the structure of psychology services at the institution. Not all patients are seen by psychology; patients are referred to psychology by the team and appointments occur in the psychology clinic and were not well-integrated within the hematology clinic visit.
Cycle 2
The second cycle addressed some of the problems identified during Cycle 1. The emotional/cognitive domain checklist was revised to reflect psychology clinic utilization (psychotherapy and testing) and a section was added where team members could indicate individualized action plans. Seventeen patients out of 18 eligible patients were assessed (94.4%): 1 patient was lost to follow-up. At the conclusion of this cycle, we found that several patients had not completed certain transition program components, such as genetic education or their PHR. Therefore, we decided that we needed to indicate this and create a Plan of Action (POA) to ensure completion of program components. The POA indicated which components were outstanding, when these components would be completed, and when the team would discuss the patient again to track their progress with program components (eg, 6 months later).