METHODS
Setting
Cincinnati Children’s Hospital Medical Center is a nonprofit pediatric medical center with 587 inpatient beds in Ohio providing acute and chronic care for children in Southern Ohio, Northern Kentucky, and Southeastern Indiana. The center’s Comprehensive Sickle Cell Center provides comprehensive care to approximately 280 children with SCD in the region from birth to 21 years of age. The medical center is the only major pediatric inpatient facility in the tri-state area. Greater than 75% of the SCD patients at our center live within a 15-mile radius, therefore, essentially all ED visits and hospitalizations for our patients occur at our center.
Participants
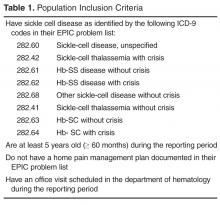
Patients were eligible for the intervention if they met the following criteria: (1) a diagnosis of SCD documented in the EMR (Epic Systems), (2) 5 years to 21 years of age, and (3) attendance of an outpatient visit in the Comprehensive Sickle Cell Center on or after January 2012 ( Table 1 ). We did not target children younger than 5 years of age because data on our patients’ ED use showed that the majority of the younger children with SCD did not have ED visits for pain only (only 6 of 132 visits during a 12-month period).
Improvement Team
The core QI team consisted of multidisciplinary health care providers with experience caring for patients with SCD, including 3 SCD nurse care managers, 2 physicians, 2 PhD psychologists, 4 nurse practitioners, a QI consultant, and a data analyst. Additional support and suggestions were received from other SCD team members (eg, social workers, school interventionists). The core QI multidisciplinary team met weekly to design and test the intervention and implementation process.
Intervention
The intervention consisted of the following elements: (1) pre-visit review to identify eligible patients needing a new or updated home pain management plan; (2) family completion of a pain assessment tool; (3) review of pain assessment tool by SCD team; (4) development of collaborative home plan with family and the medical team; (4) integration of nonpharmacological strategies into the home plan (developed with the psychologist); (5) printed copy of the plan for family to take home; (6) documentation of HPMP in the EMR ( Table 2 ); and, (7) a follow-up phone call for eligible patients with ED or urgent care visits for uncomplicated SCD pain by the nurse care manager.
Implementation
Each week the data analyst generated a list of eligible patients with ICD-9 diagnostic codes for SCD using SQL (structured query language) to extract the data from the EMR (Table 1). The SCD nurse care managers reviewed the list and notified the team of those patients needing a pain assessment and updated HPMP during the daily pre-clinic patient review rounds each morning.
The provider seeing the patient that day facilitated the patient and family’s completion of the pain assessment tool. The pain assessment tool consisted of 13 items and measured recent illnesses or transfusions, patient’s pain location, intensity, associated symptoms, potential triggers, and the impact of the pain on quality of life (missed days of school/work). In addition, the patient’s current pain management strategies, perceived effectiveness of those strategies, and analgesics available at home was recorded.