According to the policy and standard operating procedures that govern research at the Ottawa Hospital Research Institute, this work met criteria for quality improvement activities exempt from ethics review.
Intervention
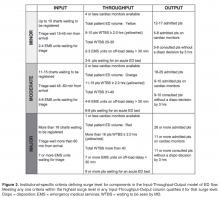
A working group comprising a project manager, ED physicians, managers, educators, care facilitators, and inpatient flow managers developed specific criteria defining various levels of surge for each component of the Input-Throughput-Output model ( Figure 2 ). Since there is no universally accepted definition of surge published in the literature, the criteria were derived from consensus of local expert/leadership opinion as starting points for this project, and refined by polling frontline workers (care facilitators) on their perceptions of what constitute ED surges. The ED care facilitator’s position is held by approximately 10 senior nursing staff who are operational experts of ED flow and management, and has no specific bedside nursing duties assigned. Its main mandate is to manage overall flow of the department including but not exclusive to communication with inpatient units and local EMS dispatch, liaising with ED physicians to facilitate efficient use of limited monitored beds and other resources, and reassigning nursing resources around the department as needed.Over a 4-day period care facilitators were polled on an hourly basis to determine what factors were important to the in determining how “busy” they perceived the ED to be. These factors included but were not limited to: total number of patients waiting to be seen; time to physician initial assessment; number of monitored beds available; and number of admitted patients boarded in the ED. Analysis was done to prospectively compare their perception of surge levels to the proposed Surge Plan metrics, and to ensure that the individual criteria for each level was practically meaningful and accurate.
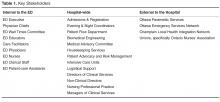
Next, a set of standardized action and response plans were developed and agreed upon that tied specifically to a corresponding component of the different measured ED surge levels (these action plans are detailed in an online Appendix and are also available from the author). The fundamental guiding principles behind the development of each action item was that it should (1) target underlying causes - in a standardized way - specific to the relevant Input-Throughput-Output surge, (2) provide escalating level of effectiveness for each corresponding escalation in the surge level (eg, contacting a staff physician directly for a disposition decision for patents consulted in the ED, if the resident trainees have failed to do so in a timely manner), and (3) coordinate actions by various stakeholders in a planned and organized manner. Practically, the standardized targeted actions span across 5 different roles, which were explicitly listed on action sheets for care facilitators, clinical managers, patient flow managers, evening and night coordinators, and clinical directors.