The 2015 National Lipid Association (NLA) released “Part 1” guidelines for the management of dyslipidemia and then provided “Part 2” about a year later, which focuses on management for special populations. To summarize, the NLA guidelines recommend that elderly patients between the ages of 65 and 80 receive a high-intensity statin for secondary prevention after special consideration of the potential risks and benefits. In patients over the age of 80, NLA recommends a moderate-intensity statin for secondary prevention. For primary prevention, NLA recommends utilizing the pooled cohort risk equation to analyze patient characteristics, keeping in mind that age is a driving factor for increased risk of CVD and that the actual risk for developing a CV event may be “overestimated” if the patient has no other risk factors other than their age. When evaluating patients between the ages of 65 and 79 for primary prevention, NLA suggests following Part 1 of the guidelines. In Part 1, NLA recommends evaluating the patient’s characteristics and suggests a moderate- or high-intensity statin if the patient is considered “very high risk” or “high risk” and a moderate-intensity statin for patients who are considered “moderate risk”. For patients over the age of 80, they recommend utilizing a moderate- or a low-intensity statin depending on frailty status or if significant comorbidities or polypharmacy exist [13,14].
In 2017, the American Association of Clinical Endocrinologist (AACE) released guidelines for the management of dyslipidemia and CVD prevention. AACE recommends that patients over age 65 be screened for dyslipidemia, and those who have multiple risk factors, other than age, should be considered for treatment with lipid-lowering therapy. AACE focuses on specific target LDL-C levels as treatment goals [15].
In addition to statins, other lipid-lowering therapies are used to treat dyslipidemia. The 2016 American College of Cardiology (ACC) Task Force reported on the use of non-statin therapies for the management of dyslipidemia and prevention of clinical ASCVD [16]. The committee concluded that ezetimibe added to statin therapy, bile acid sequestrants as monotherapy, and niacin as monotherapy all have some benefit for the prevention of clinical ASCVD. These guidelines also discuss the use of PCSK-9 inhibitors and their potential to decrease the risk of clinical ASCVD, but trials are currently ongoing to determine actual benefit. These guidelines address special populations but they do not consider the elderly in their recommendations. Currently, the only special populations included are patients with heart failure, those on hemodialysis, women who are of childbearing age or pregnant, and those with autoimmune diseases [16]. The literature available for each individual medication is discussed in further detail below.
Evidence for Secondary Prevention
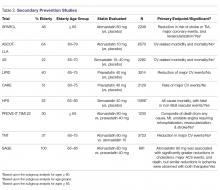
The benefits of statin therapy for secondary prevention in the elderly is more established than it is for primary prevention (Table 2).
SPARCL (Stroke Prevention by Aggressive Reduction in Cholesterol Levels), published in 2006, evaluated atorvastatin 80 mg for secondary ASCVD prevention in patients > 18 years with recent stroke or TIA ( 65 years) compared to younger patients. Unfortunately, no difference in the primary outcome was found, but secondary endpoints (reduction in risk of stroke or TIA, major coronary events, and revascularization) were significantly reduced in the elderly age group [17,18].The ASCOT–LLA (Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm), published in 2003, evaluated the effect of atorvastatin 10 mg on reducing ASCVD events in moderate-risk patients between 40–79 years of age who had hypertension and normal or slightly elevated LDL-C levels, with at least 2 other risk factors for CVD (age > 55 years was considered a risk factor). The primary outcome was non-fatal MI including silent MI and fatal CHD. A significant reduction was seen in the primary endpoint. Over half of the study population was > 60 years of age, with a mean age of 63 years. In a post-hoc analysis, stroke prevention was found to be similar in patients who were > 70 years of age and those < 70 years of age [19].
One of the first trials to specifically analyze the impact of age on lipid-lowering therapy in secondary ASCVD prevention was the Scandinavian Simvastatin Survival Study (4S), published in 1994. They evaluated the effect of simvastatin 20 mg on CV-related mortality and morbidity in patients 35–70 years of age with hyperlipidemia and a history of angina or acute MI occurring > 6 months of the study starting. The primary outcome was all-cause mortality. The secondary endpoint was time to first major CV event, which included coronary death, non-fatal acute MI, resuscitated cardiac arrest, and silent MI. Simvastatin significantly reduced the primary outcome and CHD-related deaths. A subgroup analysis of the study population > 60 years of age showed that age made no significant impact on primary or secondary outcomes; however, investigators noted that these subgroup analyses had less statistical power than the population as a whole [20].
Published in 1998, the LIPID (Long-Term Intervention with Pravastatin in Ischemic Disease) study evaluated the effects of pravastatin 40 mg daily on CHD-related mortality and overall mortality in patients with hyperlipidemia and clinical ASCVD (previous MI or unstable angina). The primary outcome observed was fatal CHD. Pravastatin significantly reduced the primary outcome, overall mortality, and pre-specified CV events. In a subgroup analysis, age group ( 65, and > 70 years) had no significant impact on the combined outcome of death from CHD and nonfatal MI; however, patients 65 to 70 years of age made up less than half of the study population [21].
The Cholesterol and Recurrent Events (CARE) trial, published in 1996, looked at the effect of pravastatin 40mg therapy for secondary ASCVD prevention following an MI in patients who had average cholesterol levels (defined as TC < 240 mg/dL and LDL-C 115–174 mg/dL). The primary endpoint assessed was time to fatal CHD or nonfatal MI. To meet statistical power they looked at subgroups for a broader outcome of a major coronary event (including fatal CHD, nonfatal MI, bypass surgery, and angioplasty). Pravastatin significantly reduced the primary outcome. The significant reduction in coronary events produced by pravastatin was noted to be significantly greater in women and in patients with higher pretreatment levels of LDL-C, but was not significantly impacted by age group (24–59 vs. 60–75 years) [22].
The Heart Protection Study (HPS), published in 2002, looked at the long-term effects of lowering LDL-C with simvastatin 40 mg in patients 40 to 80 years of age at high risk for mortality due to either vascular or nonvascular causes. The primary outcome assessed was all-cause mortality, with fatal or nonfatal vascular events as co-primary outcomes for subcategory analyses. Simvastatin significantly reduced both primary and co-primary outcomes, but there was no significant difference when they looked at nonvascular mortality between groups. Neither age nor baseline LDL levels were reported to have had a significant impact on outcomes. Over half the population was > 65 years of age, and about one-third of the population was > 70 years of age [23].
The PROVE-IT/TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy–Thrombolysis in Myocardial Infarction 22) trial, published in 2004, compared pravastatin 40 mg (moderate-intensity) to atorvastatin 80 mg (high-intensity) for secondary ASCVD prevention in patients with recent acute coronary syndrome (ACS) 65 years of age and the mean age was 58 years [24].
The TNT (Treating to New Targets) trial, published in 2005, looked at secondary ASCVD prevention in regards to targeting LDL-C levels to < 100 mg/dL or < 70 mg/dL with atorvastatin 10 mg and atorvastatin 80 mg. Patients had stable coronary artery disease (CAD) and baseline LDL-C levels < 130 mg/dL. The primary endpoint was the occurrence of a CV event (CAD mortality, nonfatal MI not related to procedure, resuscitation after cardiac arrest, or fatal or nonfatal stroke). High-intensity atorvastatin (80 mg) significantly reduced the primary outcome. The mean age of the study population was approximately 61 years. The study reported no statistical interaction for age or sex in the primary outcome measure [25].
The Study Assessing Goals in the Elderly (SAGE), published in 2007, evaluated the effects of pravastatin 40 mg (moderate-intensity) vs atorvastatin 80 mg (high-intensity) on secondary ASCVD prevention in patients 65 to 85 years (mean age 72) with stable CHD, LDL-C 100–250 mg/dL, with at least 1 episode of myocardial ischemia with total ischemia duration > 3 minutes. The primary efficacy outcome observed was absolute change in total duration of myocardial ischemia on 48-hour ambulatory electrocardiographic monitoring from baseline to month 12. No significant difference was observed in efficacy between the two groups for the primary endpoint, but the intensive statin therapy group showed greater benefit respective to several secondary outcomes, including major acute CV events and death [26].
In summary, while these trials provide evidence that statin therapy is beneficial in a wide range of patients with clinical ASCVD and dyslipidemia, the trial data does not provide definitive guidance for treating elderly patients at this time. Given the small percentage of elderly patients that were included, some of the trial results reporting statistical significance in this age group hold less clinical significance. It appears that high-intensity statin therapy was more likely to effectively prevent clinical ASCVD and death than moderate-intensity statin therapy, but more evidence is needed regarding secondary prevention in patients over age 75.