Deep surgical-site infections (SSIs) and septic arthritis are not uncommon after the surgeries for periarticular knee fractures, a meta-analysis of existing research found.
A smaller analysis of 1,567 patients found that 2.4% had septic arthritis. “Surgeons managing periarticular knee fractures should be vigilant when wounds are not pristine,” the investigators recommended.
The report, which appeared in JAMA Network Open, was led by premed student Grayson R. Norris of High Point (N.C.) University.
The researchers noted that there are widely variable statistics regarding SSI after surgery for periarticular knee fractures. A better understanding of the risk would help orthopedic surgeons, given the mortality risk and extra costs associated with postoperative deep SSIs.
For the analysis, the researchers reviewed 117 studies with 11,432 patients who had fractures in the tibial plateau (61% of studies), distal femur (14%), proximal tibia (11%), patella (9%), and multiple sites (6%). More than two-thirds of the studies were retrospective.
Overall, 5.7% of patients suffered deep SSIs, with the highest percentage in the proximal tibia group (6.4%).
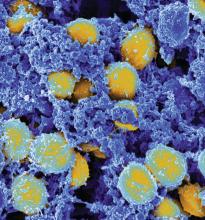
A total of 20 studies examined septic arthritis and found that 2.4% of patients in those studies suffered from the condition. Of 182 cases of deep SSIs with bacterial culture results, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus were the most common bacteria.
“Considering that MRSA was the most common pathogen in our study and that this pathogen is increasing in prevalence, health care practitioners should revisit the use of specific and appropriate prophylactic antibiotics,” the researchers wrote. “Risk factors, such as open fractures, diabetes, smoking, and, most importantly, compartment syndrome, should alert the treating surgeon to an increased risk. Further work is needed to mitigate the association of these conditions with SSI risk in periarticular knee fractures.”
The researchers added that many of the studies in their analysis were of poor quality. “Authors in orthopedic traumatology should strive to conduct higher-quality research, such as randomized clinical trials and case-control or cohort studies,” they noted.
One author reported receiving grants from Zimmer Biomet and DePuy Synthes outside the submitted work. No other disclosures were reported. No study funding was reported.
SOURCE: Norris GR et al. JAMA Netw Open. 2019;2(8):e199951.