At least 24 people in the northeast United States have been infected with a newly described, as-yet-unnamed, tick-borne illness.
Borrelia miyamotoi is a spirochete related to Borrelia burgdorferi, the microorganism that causes Lyme disease, and is transmitted by the same four tick species that carry B. burgdorferi. In a case series of 875 patients, B. miyamotoi was present in 1% of healthy people who lived in a Lyme-endemic area, 3% of those with suspected Lyme, and 21% of those with a warm-weather viral-like illness in the late spring or summer, who attended a Lyme screening clinic.
Eighteen of the cases plus an additional one are described in two reports published in the Jan. 17 issue of the New England Journal of Medicine. These occurred in Connecticut, New York, and Rhode Island; one was in New Jersey. Since these cases were described, five additional patients have been confirmed, according to a spokesperson for Imugen, the Norwood, Mass., laboratory that performed immunoassays on some of the patients. Those were in Massachusetts, New Jersey, Connecticut, and New York.
There is reason to believe that patients can be coinfected with both B. miyamotoi and B. burgdorferi, and that ticks can harbor both simultaneously, said Dr. Peter Krause, an epidemiologist at Yale School of Public Health, New Haven, Conn., and primary author of one of the papers (N. Engl. J. Med. 2013 Jan. 17 [doi:10.1056/NEJMc1215469]).
But because the spirochetes are genetically similar, the illnesses they cause respond to the same antibiotic regimen, Dr. Krause said in an interview.
B. miyamotoi was first identified in Japan in 1995. In 2001, another Yale epidemiologist, Durland Fish, Ph.D., found it in 2.5% of tick nymphs collected in Maryland. In 2011, Dr. Krause and Dr. Fish together identified the first human cases – a series of 46 patients in Russia.
Dr. Krause reviewed serum samples collected from 1990 to 2010: 584 from healthy subjects who lived in Lyme-endemic areas and participated in a serotyping survey; 277 from the group with suspected Lyme disease; and 14 from those who presented at the Lyme clinic.
Four of the 18 positive subjects had reported the typical erythema migrans skin lesion. Two others had an atypical smaller-sized lesion – less than 5 cm in diameter. The rest had no reported rash.
Three patients were actually negative for B. miyamotoi during their acute illness, but showed seroconversion during their recovery. This indicates that B. miyamotoi probably did not cause the initial illness, suggesting coinfection with B. burgdorferi.
One of these patients was quite ill, according to the report. This patient had no skin lesion and no evidence of human granulocytic anaplasmosis coinfection. He showed a fever of more than 39 degrees Celsius, headache, neck stiffness, fatigue, myalgia, arthralgia, abdominal pain, cough, sore throat, and right inguinal lymphadenopathy. This patient recovered after a 14-day course of doxycycline; all of the other symptomatic patients treated with standard doxycycline or amoxicillin treatment also recovered.
None of the cases in Dr. Krause’s cohort showed any serious neurologic symptoms. However, the single patient reported from New Jersey – an immunocompromised 80-year-old women – did.
This woman was treated in 2011, Dr. Joseph L. Gugliotta and colleagues reported. She had experienced 4 months of declining mental status, including increasing confusion; withdrawal from family interactions; episodes of staying in bed; unstable gait; hearing problems; and a 30-pound weight loss and decreased appetite. She also had a recent diagnosis of depression, wrote Dr. Gugliotta, an infectious disease specialist in Flemington, N.J. (N. Engl. J. Med. 2013 Jan. 17 [doi:10.1056/NEJMoa1209039]).
The patient had been treated for non-Hodgkin’s lymphoma during 2005, and was still taking rituximab every 6 months.
She did not report having any recent tick bites, and had no typical Lyme rash. However, she had been treated for Lyme disease twice in the past, in 2006 and 2007, when she did present with the rash. She lived in a rural setting in a Lyme-endemic area.
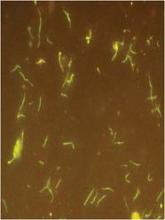
The initial exam showed no new oncologic activity and no structural brain problems. A lumbar puncture showed pleocytosis. However, "an extraordinary density of morphologically distinct spirochetes" later identified as B. miyamotoi were found in CSF sediment, the authors noted.
The patient did not respond well to an initial infusion of ceftriaxone, developing a fever and low systolic blood pressure. She then received a 30-day course of 24 million units intravenous penicillin G. Her symptoms began to improve after 5 days of treatment. By the end of the regimen, she had returned to normal, Dr. Gugliotta and his coauthors said.