The shortage of adult and child neurologists in the United States is set to go from bad to worse, according to a simulation study sponsored by the American Academy of Neurology.
The demand for neurologists already exceeds the supply by about 11% overall. But by 2025 the difference between supply and demand is expected to hit 19% as Americans age and as more people have access to insurance through the Affordable Care Act.
The result of the shortfall is likely to be more of what physicians and patients are already experiencing: long wait times to get an appointment, difficulty hiring new neurologists, and large numbers of neurologists who will not accept Medicaid. Already the average wait time for a new patient to see a neurologist is 34.8 business days. In child neurology, the average wait time is 45 business days.
Officials at the American Academy of Neurology (AAN) are taking the findings to Capitol Hill in the hope of getting some legislative relief that could help improve access to neurology services.
One solution they are proposing is to increase the payment for evaluation and management codes under the Medicare payment system. Undervalued cognitive care services are part of the reason that medical students and residents, who are burdened with significant educational debt, sometimes shy away from careers in neurology, Dr. Timothy A. Pedley, AAN President, said in an interview.
"This is a problem that will only increase in magnitude unless something is done to reverse this trend," Dr. Pedley said.
In 2012, the supply of adult and child neurologists was 16,366, but the demand was for 18,180 neurologists, a shortfall of about 11% nationally. By 2025, the supply is expected to grow to about 18,060, but the demand will hit 21,440, a shortfall of 19% nationally. The figures include both adult and child neurologists, but shortages for child neurologists alone are even more severe, according to the study.
Researchers conducted a microsimulation supply and demand model study to look at how the shortfall of neurologists was likely to change between 2012 and 2025. The model simulates the career choices of neurologists throughout their careers, taking into account deaths, retirements, new graduates, and the number of patient care hours worked. The investigators relied on several sources, including databases from the AAN and the American Medical Association. They also used data and surveys from the National Residency Match Program (Neurology 2013 April 17 [doi: 10.1212/WNL.0b013e318294b1cf]).
The researchers modeled the demand for services by taking demographic, socioeconomic, and health risk factors for a representative sample in each state. They then used that data to forecast the use of neurology services, and applied estimates of neurologist productivity. They used data from the U.S. Census Bureau and the Centers for Disease Control and Prevention to make the demand projections.
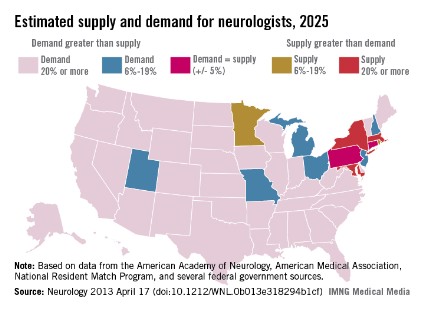
The shortage of neurologists varies by region. However, the researchers estimate that by 2025 most of the country will be facing a neurologist shortage of 20% or more, while only a few states will have enough neurologists to meet the demand.
There are several reasons for the increased demand, the researchers noted. One factor is the aging of the population and, with it, the rising prevalence of neurologic conditions. Another factor is the increased use of nonphysician providers in the primary care setting. Since these providers have limited training in neurology, there are likely to be more referrals made to neurologists.
Increased access to health insurance coverage under the Affordable Care Act also will drive demand for neurologists. The researchers estimate that it will push the projected shortfall up from 16% in 2025 to 19% overall by 2025.
The study was supported by the AAN and an educational grant from Lilly USA.