Stephanie E. MacIver, MD
Dr. MacIver will graduate residency in July 2016 and will be starting her neurophysiology fellowship at the University of South Florida.
Selim R. Benbadis, MD
Dr. Benbadis is Professor and Director of the Comprehensive Epilepsy Program at the University of South Florida and Tampa General Hospital in Tampa, Florida.
A 35-year-old right-handed woman with anxiety has a five-year history of possible syncopal events associated with pronounced tachycardia, which occur about twice a month. The events are preceded by palpitations, anxiety, and rarely a sense of déjà vu. The patient feels that if she is able to lie down and raise her legs above her head, she can prevent a full episode from happening. If she is unable prevent the spell, then she will have altered awareness for 1 to 3 minutes and will frequently bite her lower lip. The patient also reports an isolated episode of bladder incontinence. After a spell, she may feel confused for 2 to 10 minutes. As far as she can remember, these events only occur in the daytime.
She was initially evaluated by a cardiologist who suspected a diagnosis of either orthostatic hypotension or postural orthostatic tachycardia syndrome (POTS). Her tilt-table testing was inconclusive. After she failed to respond to midodrine and metoprolol, she had an implantable loop recorder placed and was referred to a neurologist. Her routine EEG and MRI were normal. She presented no other risk factors for epilepsy; however she was started on a trial dose of Keppra (levetiracetam) 500 mg twice daily. The patient was unsure if the addition of Keppra helped, so she was referred to an epilepsy monitoring unit for further clarification.
While she was hospitalized, Keppra was withheld, which lead to her typical event. She endorsed an anxiety-provoking sensation and palpitations. On the single-lead EKG her pulse went from the 60s to the 130s. She tried to stop the event by lying down and propping her feet on the railing at the foot of the bed. Initially, she was able to respond to nursing staff promptly, but as the duration of the event continued, her responses slowed yet remained appropriate. The total duration of the entire episode was 1 minute and 14 seconds. EEG demonstrated an electrographic seizure with focal onset in the right posterior hemisphere.
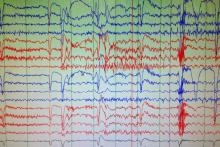
EEG at the onset of her seizure:
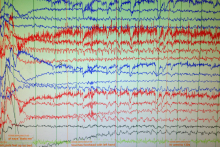
EEG evolution:
At discharge, this patient was started on the higher dose of Keppra 750 mg twice daily with the plan to increase until the events are controlled. Her cardiologist removed the loop recorder, titrated her off midodrine, and is considering reduction of metoprolol.
The correct diagnosis for this patient is focal epilepsy (right posterior hemisphere).