In this Update I highlight 5 interesting investigations on infectious diseases. The first addresses the value of applying prophylactically a negative-pressure wound dressing to prevent surgical site infection (SSI) in obese women having cesarean delivery (CD). The second report assesses the effectiveness of a preoperative vaginal wash in reducing the frequency of postcesarean endometritis. The third investigation examines the role of systemic antibiotics, combined with surgical drainage, for patients who have subcutaneous abscesses ranging in size up to 5 cm. The fourth study presents new information about the major risk factors for Clostridium difficile infections in obstetric patients. The final study presents valuable sobering new data about the risks of congenital Zika virus infection.
Negative-pressure wound therapy after CD shows some benefit in preventing SSI
Yu L, Kronen RJ, Simon LE, Stoll CR, Colditz GA, Tuuli MG. Prophylactic negative-pressure wound therapy after cesarean is associated with reduced risk of surgical site infection: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218(2):200-210.e1.
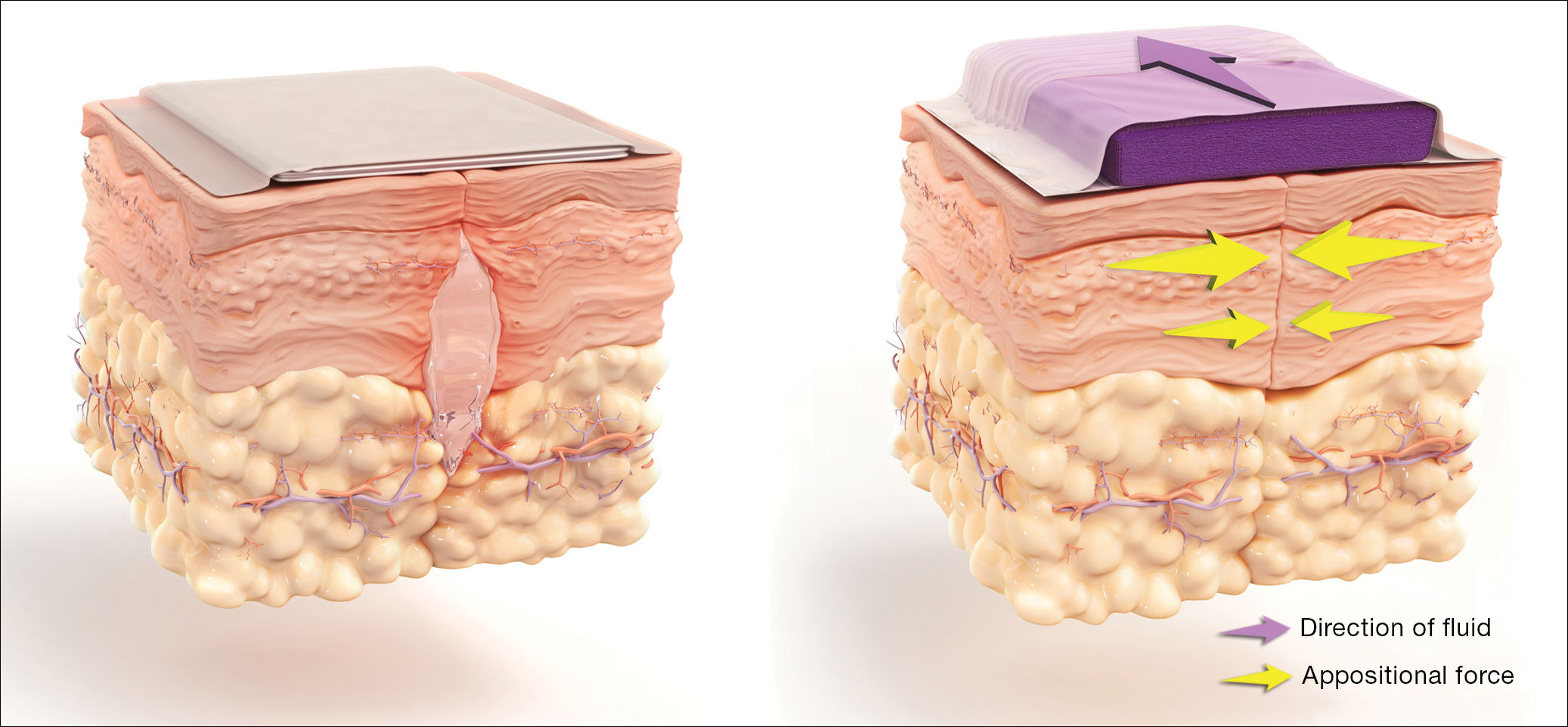
 Illustration: Used with permission. Courtesy of KCI, an Acelity Company
Illustration: Used with permission. Courtesy of KCI, an Acelity Company
Yu and colleagues sought to determine if the prophylactic use of negative-pressure devices, compared with standard wound dressing, was effective in reducing the frequency of SSI after CD.
The authors searched multiple databases and initially identified 161 randomized controlled trials and cohort studies for further assessment. After applying rigorous exclusion criteria, they ultimately selected 9 studies for systematic review and meta-analysis. Six studies were randomized controlled trials (RCTs), 2 were retrospective cohort studies, and 1 was a prospective cohort study. Five studies were considered high quality; 4 were of low quality.
Details of the study
Several types of negative-pressure devices were used, but the 2 most common were the Prevena incision management system (KCI, San Antonio, Texas) and PICO negative- pressure wound therapy (Smith & Nephew, St. Petersburg, Florida). The majority of patients in all groups were at high risk for wound complications because of obesity.
The primary outcome of interest was the frequency of SSI. Secondary outcomes included dehiscence, seroma, endometritis, a composite measure for all wound complications, and hospital readmission.
The absolute risk of SSI in the intervention group was 5% (95% confidence interval [CI], 2.0%-7.0%) compared with 11% (95% CI, 7.0%-16.0%) in the standard dressing group. The pooled risk ratio was 0.45 (95% CI, 0.31-0.66). The absolute risk reduction was 6% (95% CI, -10.0% to -3.0%), and the number needed to treat was 17.
There were no significant differences in the rate of any of the secondary outcomes other than the composite of all wound complications. This difference was largely accounted for by the difference in the rate of SSI.
How negative-pressure devices aid wound healing
Yu and colleagues explained that negative-pressure devices exert their beneficial effects in various ways, including:
- shrinking the wound
- inducing cellular stretch
- removing extracellular fluids
- creating a favorable environment for healing
- promoting angiogenesis and neurogenesis.
Multiple studies in nonobstetric patients have shown that prophylactic use of negative-pressure devices is beneficial in reducing the rate of SSI.1 Yu and colleagues' systematic review and meta-analysis confirms those findings in a high-risk population of women having CD.
Study limitations
Before routinely adopting the use of negative-pressure devices for all women having CD, however, obstetricians should consider the following caveats:
- The investigations included in the study by Yu and colleagues did not consistently distinguish between scheduled versus unscheduled CDs.
- The reports did not systematically consider other major risk factors for wound complications besides obesity, and they did not control for these confounders in the statistical analyses.
- The studies included in the meta-analysis did not provide full descriptions of other measures that might influence the rate of SSIs, such as timing and selection of prophylactic antibiotics, selection of suture material, preoperative skin preparation, and closure techniques for the deep subcutaneous tissue and skin.
- None of the included studies systematically considered the cost-effectiveness of the negative-pressure devices. This is an important consideration given that the acquisition cost of these devices ranges from $200 to $500.
Results of the systematic review and meta-analysis by Yu and colleagues suggest that prophylactic negative-pressure wound therapy in high-risk mostly obese women after CD reduces SSI and overall wound complications. The study's limitations, however, must be kept in mind, and more data are needed. It would be most helpful if a large, well-designed RCT was conducted and included 2 groups with comparable multiple major risk factors for wound complications, and in which all women received the following important interventions2-4:
- removal of hair in the surgical site with a clipper, not a razor
- cleansing of the skin with a chlorhexidine rather than an iodophor solution
- closure of the deep subcutaneous tissue if the total subcutaneous layer exceeds 2 cm in depth
- closure of the skin with suture rather than staples
- administration of antibiotic prophylaxis, ideally with a combination of cefazolin plus azithromycin, prior to the surgical incision.
Read about vaginal cleansing’s effect on post-CD endometritis