From the Editor
Why is breast density a weighty matter?
What will you tell your patient who asks about the clinical significance of dense breasts detected on her mammogram? Here I offer my current...

Letters from readers
“THE SGR IS ABOLISHED! WHAT COMES NEXT?”
LUCIA DIVENERE, MA (PRACTICE MANAGEMENT; JUNE 2015)
Do ACOG guidelines protect us from liability?
I read Ms. DiVenere’s June article with interest, but I found this point she quoted confusing: "The law protects physicians from liability from federal or state standards of care. No health care guideline or other standard developed under federal or state requirements associated with this law may be used as a standard of care or duty of care owed by a health care professional to a patient in a medical liability lawsuit."
I have 2 questions: How do you interpret the use of guidelines by the American College of Obstetricians and Gynecologists (ACOG), since they are developed independently by a specialty society rather than by federal or state “requirements”? Does this only pertain to liability lawsuits concerning billing of fees, or does it pertain to medical malpractice civil lawsuits?
In the Medicare Access and CHIP Reauthorization Act, I find this section that seems to contradict the protection1:
What is the bottom line? No law can protect and provide immunity to a physician for true medical malpractice. This federal law says “no preemption.”
Arnold D. Wharton, MD
Tyler, Texas
Reference
1. Pub L No. 114–10. Medicare Access and CHIP Reauthorization Act of 2015. 114th Congress. Title 1—SGR repeal and Medicare Provider Payment Modernization. §106. Reducing administrative burden and other provisions. 129 STAT.143. http://www.gpo.gov/fdsys/pkg/PLAW-114publ10/pdf/PLAW-114publ10.pdf. Accessed June 10, 2015.
Ms. DiVenere responds
I thank Dr. Wharton for his interesting perspective. To answer the first questions, this section of the law only applies to guidelines and standards created by a federal or state entity, not to ACOG guidelines, and is intended to provide one area of protection from medical malpractice lawsuits. Interestingly, legislation has been introduced in the US House by Congressman Andy Barr (R-KY), with ACOG’s support, to create liability safe harbors for physicians who follow care guidelines developed by their relevant specialty society.
As for the question about preemption, this section of the law allows stronger state laws to stand; this federal law would not preempt state laws.
Statute of limitations still in effect; contact your insurer
While the end result to dismiss the patient was achieved, the statute of limitations for a possible malpractice suit had not fully run. I would suggest that the physician contact his/her insurer so that they can open a file and be alerted for a possible suit. Insurers generally require physicians to notify them of any potential suits.
Lynn Frame, MD, JD
Tulsa, Oklahoma
Dr. Sanfilippo and Mr. Smith respond
Our thanks to Dr. Frame for the good reminder that physicians should always remember the obligation to inform malpractice insurance carriers when a malpractice claim is being, or may be, filed. Insurance contracts vary somewhat regarding when notice must be given.
In the hypothetical case, there was an angry patient but no formal threat of legal action. Some lawyers take the sensible position that “when in doubt, notify.” Others are reluctant to “over notify” carriers. Our view is that this is one of the areas in which it may be beneficial for a physician to have an ongoing professional relationship with an attorney to allow for advice on when to provide insurance carrier notification.
Videos show very useful techniques for malpositioned IUDs
I have placed somewhere in the ballpark of 2,000 intrauterine devices (IUDs) and have had 2 perforations that I am aware of (and probably many more malpositioned IUDs that I am unaware of). Some of those were likely the cause of a patient’s pain and were either removed or hysteroscopically repositioned. Dr. Advincula’s edited video from several cases demonstrates very useful techniques in the surgical management of these problems.
Philip Ivey, MD
Casa Grande, Arizona
What will you tell your patient who asks about the clinical significance of dense breasts detected on her mammogram? Here I offer my current...

The law repealing the sustainable growth rate not only eliminated physicians’ perennial nemesis but also preserved or enhanced other critical...

What are your legal and ethical responsibilities when you feel you need to end your relationship with a patient? The steps you take before such...
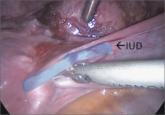
Techniques for managing intrauterine devices that have become embedded, translocated, or perforated
Nearly 100% of pregnant women infected with Ebola die. Clinicians should be aware of this statistic and familiar with general, as well as...

About 7% of 2014 graduating medical students did not get matched to a residency program for their first-choice ObGyn specialty
Contemporary data suggest that it is.
The benefit is small and the cost is high, according to this comparative modeling study.
