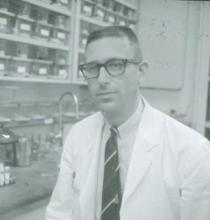
In 1966, Dr. Charles Hammond was wrapping up a 2-year stint at the National Institutes of Health where he served at the behest of the military draft board. He had graduated from medical school just 5 years prior, and was in the middle of his ob.gyn. residency training at Duke University in Durham, N.C. when he was called to serve.
His experience wasn’t unusual for the time.
“When the draft board called, you went,” he said in an interview.
When he returned, he picked up where he left off. Residencies at that time were an “open-ended thing,” sometimes lasting 5 or 6 years, depending on staffing needs and other considerations.
Dr. Hammond, now an emeritus professor at Duke, regards his public service commission as an opportunity that advanced his academic career – despite the interruption of his residency training.
Such draft-related interruptions ended in the wake of the Vietnam War, of course, but the late 1960s and the 1970s ushered in a whole new era of changes in ob.gyn. residency training programs.
By 1968, residencies lasted 4 years, and fellowships were for 2 years. Ob.gyn. subspecialties hadn’t yet been introduced, explained Dr. Sandra A. Carson, vice president for education at the American College of Obstetricians and Gynecologists.
“That is essentially how things worked for a long time,” she said in an interview.
That’s not to say there weren’t numerous other changes taking place in the specialty. In a series of interviews with physicians and educators who discussed the myriad ways that residency training has evolved over the last 50 years, a number of themes emerged.
Women in medicine
A striking change over the past 5 decades has been the increasing number of women in medicine. Nowhere has that been in greater evidence than in obstetrics and gynecology.
“There were a few – but very few,” Dr. Hammond said of women in medicine in the 1960s.
There was “a philosophy that men did it better,” he said, adding, “That has been nicely shown to be inaccurate.”
Currently, about 80% of first-year ob.gyn. residents are women, compared with 15% in 1975.
“Maybe even 83% now,” Dr. Carson said, noting that even in the early 1980s when she was in training, women were “few and far between.”
According to a 2011 workforce report by Dr. William F. Rayburn, obstetrics and gynecology has the highest percentage of women residents of any medical specialty – 80% in 2009 versus an average of 46% for other specialties combined, and that figure has remained fairly constant.
Dr. Kasandra Scales, a fourth-year resident at the State University of New York, Syracuse, said she is glad to be part of this era of the specialty where women play an integral role in the advancement of women’s health care.
“I believe our voice and unique perspective to relate with common experiences, such as the physical birth of a child or personal choices in contraception... has enhanced our specialty,” she said.
That said, the fact that men are noticeably absent from the pool of ob.gyn. applicants and residents concerns her. “There should be a balance, she said. “I think it is important to have diversity of all types in the healthcare system.”
Dr. Hammond looked back on his days in residency training and recalled pockets of resistance to the increasing number of women in medicine, but the ultimate effect was good for the specialty, he said, explaining that the quality of the resident pool improved steadily, because the number of qualified candidates increased.
“It has been an interesting interval to watch,” he said, specifically mentioning the demands that women faced in terms of family obligations, childbirth, and childrearing.
Restrictions on work hours instituted in residency programs in more recent years may have played an important role in opening the door to more women, he said.
Work hours down, learning curve up
Dr. Carson agreed that work-hour restrictions instituted in 2003 and updated in 2011, which cap the work week at 80 hours and also apply limits on shift hours, likely encouraged more women to enter the field. One constant over the last 50 years is the biological clock, she said, explaining that the pressures and demands of residency before limits were put in place may have steered women away.
Work-hour restrictions provide more flexibility, but they aren’t without controversy.
Dr. Hammond said he sees the value in work hour restrictions, but working long hours as a resident – sometimes as many as 110 hours per week – had its benefits, too.