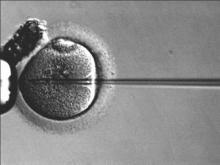
HELSINKI, FINLAND – Serum anti-Müllerian hormone levels do not predict clinical pregnancy, according to findings from a retrospective cohort study of patients undergoing intra-cytoplasmic sperm injection.
Indeed, although serum anti-Müllerian hormone (AMH) levels are closely related to female age and are a robust marker of ovarian reserve and ovarian response to gonadotropins, even patients with very low serum AMH levels in the study had a reasonable reproductive outcome, Alberto Pacheco Castro, PhD, of IVI Madrid, reported at the annual meeting of the European Society of Human Reproduction and Embryology.
The positive correlation between serum AMH and ovarian responses is well known, but there has been no consensus about whether ovarian stimulation should or should not be recommended for infertile women with low AMH values, he said. The new findings suggest that serum AMH levels should not be used to guide decision-making about ovarian stimulation in infertile women.
In the study, 5,570 intracytoplasmic sperm injection (ICSI) cycles between 2008 and 2014 were evaluated. No differences were seen in implantation rates or spontaneous abortion rates across six patient groups classified according to AMH levels. The groups had AMH levels less than or equal to 0.21 mg/mL, 0.22-0.8 ng/mL, 0.81-1.7 ng/mL, 1.71-3.2 ng/mL, 3.21-5.39 mg/mL, and greater than or equal to 5.40 mg/mL, respectively; the corresponding implantation rates were 28.9%, 25%, 29%, 28.8%, 30.5%, 35.3%, and the corresponding spontaneous abortion rates were 27.9%, 26.8%, 31%, 28.8%, 25.7%, and 22.1%, Dr. Pacheco said.
The clinical pregnancy rates in the groups were 45.3%, 48.1%, 47.4%, 45.2%, 48.0%, and 54.1%, respectively. Although the clinical pregnancy rates differed significantly between the highest and lowest AMH level groups, even the groups with the lowest levels had relatively good clinical pregnancy rates, and the receiver operating characteristic (ROC) curve showed no predictive value of AMH levels for clinical pregnancy, he noted.
The study comprised women from a university-affiliated infertility clinic, and their AMH levels were measured with a commercial test kit. Cycles were performed after controlled ovarian stimulation, pertinent data were collected for each cycle, and clinical results after embryo transfer were recorded.
The groups as classified by AMH levels differed significantly (lowest vs. highest level groups) with respect to age (mean age of 39 years vs. 36 years), antral follicle count (1.93 vs. 6.35), follicle-stimulating hormone dose (1606 IU vs. 1392 IU), oocytes retrieved (2.9 vs. 14), and mature oocytes (2.9 vs. 14.0), but not with respect to years of sterility, body mass index, or days of stimulation.
However, the study is limited by its retrospective design – it is possible that patients with very low AMH levels decided against ovulation stimulation – thus, prospective validation of the findings is required, Dr. Pacheco said.
He reported having no disclosures.