During vaginal delivery spontaneous perineal trauma and extension of episiotomy incisions are common. A severe perineal laceration that extends into or through the anal sphincter complex is referred to as an obstetric anal sphincter injury (OASIS) and requires meticulous repair. Following the repair of an OASIS, serious wound complications, including dehiscence and infection, may occur. In Europe the reported rate of OASIS varies widely among countries, with a rate of 0.1% in Romania, possibly due to underreporting, and 4.9% in Iceland.1 In the United States the rates of 3rd- and 4th-degree lacerations were reported to be 3.3% and 1.1%, respectively.2
Risk factors for OASIS include forceps delivery (odds ratio [OR], 5.50), vacuum-assisted delivery (OR, 3.98), and midline episiotomy (OR, 3.82).3 Additional risk factors for severe perineal injury at vaginal delivery include nulliparity (adjusted odds ratio [aOR], 2.58), delivery from a persistent occiput posterior position (aOR, 2.24), and above-average newborn birth weight (aOR, 1.28).4
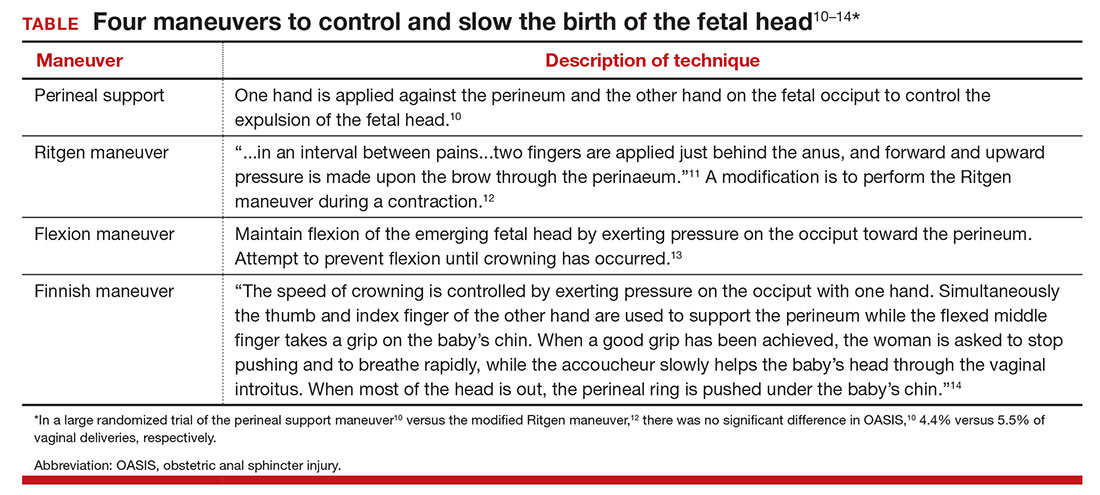
In a meta-analysis of randomized trials, the researchers reported that restrictive use of episiotomy reduced the risk of severe perineal trauma (relative risk [RR], 0.67) but increased the risk of anterior perineal trauma (RR, 1.84).5 The American College of Obstetricians and Gynecologists (ACOG) recommends that episiotomy should not be a routine practice and is best restricted to use in a limited number of cases where fetal and maternal benefit is likely.6 In addition, ACOG recommends that if episiotomy is indicated, a mediolateral incision is favored over a midline incision. In my practice I perform only mediolateral episiotomy incisions. However, mediolateral episiotomy may be associated with an increased risk of postpartum perineal pain and dyspareunia.7 Use of warm compresses applied to the perineum during the second stage of labor may reduce the risk of 3rd- and 4th-degree lacerations.8 Techniques to ensure that the fetal head and shoulders are birthed in a slow and controlled fashion may decrease the risk of OASIS.9 See the TABLE, “Four maneuvers to control and slow the birth of the fetal head.”10–14
Related article:
Stop performing median episiotomy!
Wound complications following the repair of a 3rd- or 4th-degree laceration are reported to occur in approximately 5% to 10% of cases.15 The most common wound complications are dehiscence, infection, abscess formation, pain, sexual dysfunction, and anal incontinence. Minor wound complications, including superficial epithelial separation, can be managed expectantly. However, major wound complications need intensive treatment.
In one study of 21 women who had a major wound complication following the repair of a 4th-degree laceration, 53% had dehiscence plus infection, 33% had dehiscence alone, and 14% had infection alone.16 Major wound complications present at a mean of 5 days after delivery, with a wide range from 1 to 17 days following delivery.17 In a study of 144 cases of wound breakdown following a perineal laceration repair, the major risk factors for wound breakdown were episiotomy (aOR, 11.1), smoking (aOR, 6.4), midwife repair of laceration (aOR, 4.7), use of chromic suture (aOR, 3.9), and operative vaginal delivery (aOR, 3.4).18 In one study of 66 women with a wound complication following the repair of a 3rd- or 4th-degree laceration, clinical risk factors for a wound complication were cigarette smoking (OR, 4.04), 4th-degree laceration (OR, 1.89), and operative vaginal delivery (OR, 1.76).19 The use of intrapartum antibiotics appears to be protective (OR, 0.29) against wound complications following a major perineal laceration.19