 Illustration: Kimberly Martens for OBG Management
Illustration: Kimberly Martens for OBG Management
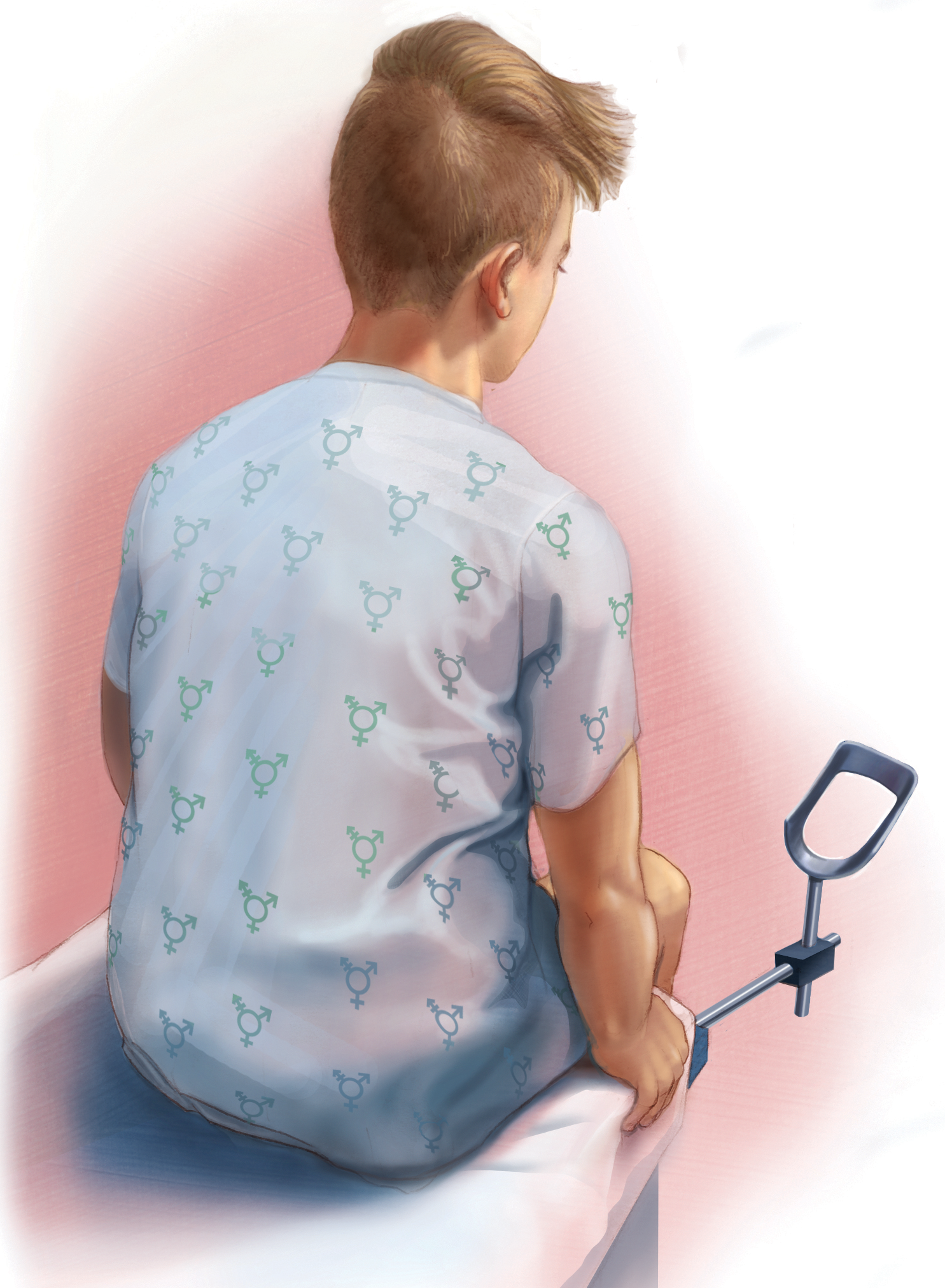
The transgender man - a female-assigned person who self-identifies as male - has unique health care needs that can be addressed only be a gynecologist. It is important to become comfortable with and educated about these health needs and their subtleties, starting with understanding the patient's gender dysphoria associated with the gynecologic visit and examination.
CASE: Transgender man consults gynecologist for fertility options
A 36-year-old transgender man considering the possibility of having his own biological children presents to the gynecology office to discuss hysterectomy as gender dysphoria treatment as well as his fertility preservation options. He has never had a gynecologic examination. Since age 24, he has been on testosterone therapy. Although his menses initially ceased, each month over the past 2 years he has had breakthrough spotting lasting 2 to 4 days, sometimes accompanied by pelvic pain and cramping. These symptoms have caused him distress and anxiety, which have led to his missing work 1 to 3 days each month. On presentation, he appears anxious and makes little eye contact. His girlfriend of 6 years has come in with him and is very supportive.
Over the past decade, transgender health care has moved to the forefront of the medical conversation. At many prominent medical centers across the United States, clinicians are forming multidisciplinary teams to help improve the health care of this patient population. Outcomes are being studied, and the literature is becoming more robust.
People tend to think of transgender women—male-assigned persons who self-identify as female—as the typical prototype for transgender people, but this focus is skewed in both society and the medical community. Transgender men—female-assigned persons who self-identify as male—remain underrepresented, mostly because they want to stay “under the radar,” especially with respect to medical care and, more specifically, routine gynecologic care.
Although the transgender woman has unique health needs and may present to a gynecologist for care after gender-affirmationsurgery, the transgender man’s many health care needs and their subtleties can be addressed only by a gynecologist. In this article, I review these intricacies of care to help increase clinician comfort in treating these patients.
Clinicians can take steps to:
- ensure all patients have the correct identifiers in their medical records
- provide staff with the proper education and diversity training
- instruct staff in proper use of pronouns
- set up unisex or gender-nonbinary restrooms with appropriate signage
- make the decor gender nonspecific.
Beth Cronin, MD, a practicing general gynecologist in Providence, Rhode Island, says that you also should consider a general sign, placed in a highly visible area, that represents your nondiscrimination policy. The AMA offers this wording: "This office appreciates the diversity of human beings and does not discriminate based on race, age, religion, ability, marital status, sexual orientation, sex or gender identity." She also recommends having education and marketing materials with affirmative imagery and content and providing educational brochures on transgender health topics.
Why transgender patients may delay seeking health care
Transgender patients remain underserved because of the health care barriers they encounter. Factors contributing to poor access include lack of health insurance, inability to pay for services, clinician insensitivity and hostility, and fear of exposure of transgender status during health care encounters.1 In a recent large survey study, 30% of transgender respondents indicated that they delayed or did not seek medical care as a result of discrimination, and those who had needed to teach their clinicians about transgenderism were 4 times more likely to postpone or not seek care.2
In a 2015 survey of ObGyns’ current knowledge and practice regarding LGBT (lesbian, gay, bisexual, transgender) care, only one-third of respondents indicated they were comfortable caring for transgender patients.3 In addition, only one-third indicated being knowledgeable about the steps transgender patients must take to transition to their self-identified gender, and less than half were familiar with the recommendations for the routine health maintenance and screening of these patients.
Much of this discomfort derives from the lack of incorporation of LGBT-specific topics in medical curricula. In 2011, Obedin-Maliver and colleagues found that, at 176 US and Canadian allopathic and osteopathic medical schools, the median time dedicated to LGBT health care needs and related topics was unsatisfactory.4 This deficiency is slowly being reduced with changes in the curricula of many health care specialties. In ObGyn residency programs, for example, transgender-specific questions have been added to annual in-service examinations. The hope is that, as education initiatives improve, clinicians will become more comfortable caring for gender-minority patients, who with improved access to care will no longer need to seek subspecialists in transgender services.
Read about the need for gyn exams, managing benign disorders, and cervical cancer screening


