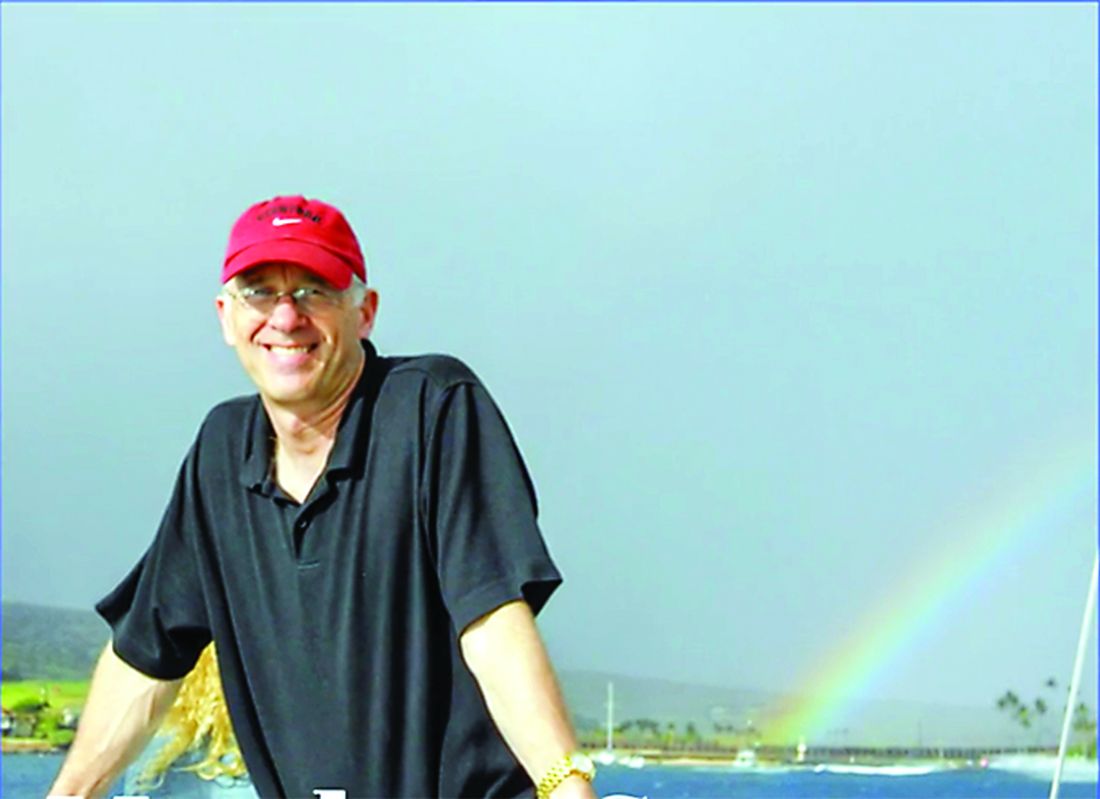
After 3 decades of caring for critical patients and managing the frenzy of bustling emergency departments, Matthew E. Seaman, MD, was ready for a calmer, slower pace.
An accomplished physician, instructor, and author, Dr. Seaman completed his final ED shift on Jan. 22, 2017, and eagerly entered a new era – retirement. He planned to travel with his wife and spend time at their tree farm near the Nisqually River in west-central Washington state, where the Seamans found solace planting Douglas firs, digging trails, and collecting driftwood.
“When people asked him what he did for a living, he said, ‘I’m a tree farmer,’ ” remembered Linda Seaman, MD, a family physician and Dr. Seaman’s wife of 30 years. “He was an avid gardener and a woodworker. He taught himself to make beautiful furniture, frames, and bowls. His amazing, handcrafted frames reflect the kind of person he was – detailed, creative, and patient.”
Dr. Matt Seaman’s retirement idyll, however, was cut short by a complaint to the Washington Medical Commission (WMC). The investigation and scrutiny that resulted, followed by a lawsuit and grueling litigation process, eroded his mental health and triggered an unyielding sense of hopelessness, family and friends say. As the legal case continued and his mental state worsened, his wife tried desperately to get her husband the mental health care he needed, but the couple encountered barriers at every turn, Dr. Linda Seaman said in a series of interviews.
“I can honestly say that I’ve never personally seen anyone suffer the way I saw my husband suffering,” Dr. Linda Seaman said. “At the end, he was done. He was so tired. He just couldn’t handle it anymore.”
Dr. Matt Seaman died by suicide on March 28, 2019, at the age of 62.
A troubling problem
An estimated 400 physicians die by suicide each year, although updated research is needed, said Sidney Zisook, MD, professor of psychiatry at the University of California, San Diego, who researches physician suicide.
“The prevalence is essentially unknown,” he said in an interview. “We have estimates, but there’s no really good registry of physician suicides. [But the rate] doesn’t appear to be going down. It’s troublesome.” Two recent studies shed some light on depressed doctors and factors that may contribute to physician suicide.
Physicians who died by suicide were far more likely to have experienced job-related problems, compared with nonphysicians, but less likely to have experienced the recent death of a loved one, according to a 2013 study of 203 physician suicides (Gen Hosp Psychiatry. 2013 Jan;35[1]:45-9). Physicians who died by suicide were more likely to be older, compared with nonphysicians, and more often were married at the time of death. The mean age for physicians in the study was 59, compared with 47 for nondoctors.
In addition, physicians who died by suicide more often had a known mental illness compared with nonphysicians, yet there was no significant difference in their use of antidepressants, the study found. However, physicians who took their own lives had a dramatically higher likelihood of having benzodiazepines and barbiturates in their systems at the time of death.
Another review involving 129,000 medical students in 47 countries found that 27% of medical students reported depression or depressive symptoms and 11% of students reported suicidal ideation during medical school. The 2016 analysis, published in JAMA, found that only 16% of students who screened positive for depression sought treatment (2016;316[21]:2214-36).
A significant portion of doctors who die by suicide never sought help from mental health specialists, primary care physicians, or even pastoral leaders, said Michael F. Myers, MD, professor of clinical psychiatry at State University of New York, Brooklyn, and the author of “Why Physicians Die by Suicide: Lessons Learned From Their Families and Others Who Cared” (2017). Shame, anxiety, and embarrassment frequently keep them from reaching out, Dr. Myers said.
Physicians who do seek care, meanwhile, often receive suboptimal care from fellow doctors, he said.
“There are a number of doctors dying by suicide each year who are dying of treatable illnesses,” said Dr. Myers, who lost a medical school roommate to suicide. “Too many doctors are falling through the cracks and not getting the kind of care that they deserve or that is state of the art.”