Intrauterine pregnancy
While excluding EP is critical, it is equally important to diagnose an IUP as expeditiously as possible to avoid inadvertent, destructive intervention. Diagnosis and management of a PUL can involve endometrial aspiration, which would interrupt an IUP and should be avoided until the possibility of a viable IUP has been eliminated in desired pregnancies. The inadvertent administration of methotrexate, a known teratogen, to a patient with an undiagnosed viable IUP can result in miscarriage, elective termination, or a live-born infant with significant malformations, all of which expose the administering physician to malpractice litigation.16,17
In desired pregnancies, it is essential to differentiate between a viable IUP, a nonviable IUP, and an EP to guide appropriate management and ensure patient safety, whereas exclusion of EP is the priority in undesired pregnancies.
Tools for diagnosing pregnancy location
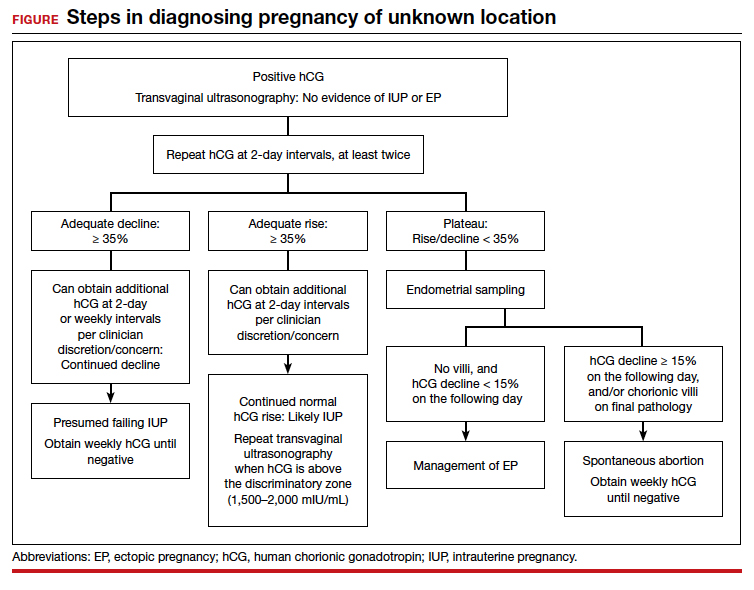
For diagnosing pregnancy location, serial hCG measurement, transvaginal pelvic ultrasonography, and outpatient endometrial aspiration are all relevant clinical tools. Pregnancy location can be diagnosed with either direct visualization of an IUP or EP by ultrasonography or with confirmed pathology (chorionic villi or trophoblast cells) from endometrial aspiration (FIGURE). A decline in hCG to an undetectable level following endometrial aspiration also is considered sufficient to diagnose a failed IUP, even in the absence of a confirmatory ultrasonography.
Trending hCG values
In stable patients with PUL, serum hCG levels are commonly measured at 2-day intervals, ideally for a minimum of 3 values. Conventional wisdom dictates that in viable IUPs, the hCG level should roughly double every 2 days. However, more recent data suggest that the threshold for minimum expected hCG rise for an ongoing IUP should be far lower when the pregnancy is desired.18 A less conservative cutoff can be considered when a pregnancy is not desired.
In a multisite cohort study of 1,005 women with PUL, a minimum hCG rise of 35% in 2 days captured the majority of IUPs, with a negative predictive value of 97.2% for IUP.19 Of note, although the cutoff of 35% was selected to reduce the risk of misdiagnosing an IUP as an EP, 7.7% of IUPs (and 16.8% of EPs) were still misclassified, showing that hCG trends must be interpreted in the context of other clinical data, including ultrasonography findings and patient symptoms and history.
A follow-up study demonstrated that hCG rises are lower (but still within this normal range) when the initial hCG value is higher, particularly greater than 3,000 mIU/mL.20
Studies show that the rate of spontaneous hCG decline in failing IUPs ranges from 12% to 47% in 2 days, falling more rapidly from higher starting hCG values.19,21 In a retrospective review of 443 women with spontaneously resolving PUL (presumed to be failing IUPs), the minimum 2-day decline in hCG was 35%.22 Any spontaneous hCG decline less than 35% in 2 days in a PUL should raise physician concern for EP.
Conversely, EPs do not demonstrate predictable hCG trends and can mimic the hCG trends of viable or failing IUPs. Although typically half of EPs present with an increasing hCG value and half present with a decreasing hCG value, the majority (71%) demonstrate a slower rate of change than either a viable IUP or a miscarriage.11 This slower change (plateau) should heighten the clinician’s suspicion for an EP.
Continue to: Progesterone levels...