Pregnancies involving multiple births are an increasingly prevalent phenomenon in most obstetrical practices, with twin gestations now accounting for more than 3% of all births in the United States.
The incidence of twinning is attributable to two main social factors: older maternal age at childbirth, which is responsible for a third of the increase, and the increased use of assisted reproductive technology (ART), which is responsible for the other two-thirds.
Although refinements in ART and recommendations to limit the number of embryos transferred during in vitro procedures have led to reductions in the number of higher-order multiples, twin gestations are still common, occurring in up to one-third of IVF pregnancies. Ovulation induction, which is a much more commonly used ART procedure, is also associated with twinning rates of 5%-10%.
What must be appreciated is the reality that twin gestations carry significant risks and contribute disproportionately to our national rates of perinatal morbidity and mortality. Although twin gestations represent just over 3% of all live births, they account for 15% of all early preterm births and 25% of all very-low birth weight infants.
Approximately 15% of all neonates with respiratory distress syndrome are twins, and twins account for 12% of all cases of grade III or IV intraventricular hemorrhage. Of all neonatal deaths in the United States, approximately 15% are twins. Moreover, approximately 10% of all stillbirths in the United States are twins.
In short, twin gestations are one of the most common high-risk conditions in obstetrical practice. Twin pregnancies are usually exciting for parents and their families, but it is important to reflect on the significant risks they can present, and to consider how these pregnancies can be optimally managed in order to reduce these risks.
No Simple Diagnosis
The first step in the optimal management of twins is to make the early diagnosis of chorionicity. The American Journal of Obstetrics & Gynecology ran a striking editorial about the significance of establishing chorionicity by first-trimester ultrasound in multiple gestations. The editorial’s authors, Dr. Kenneth J. Moise Jr. and Dr. Anthony Johnson, reflected on a talk given by Dr. Krypos Nicolaides of King’s College London, in which he broke away from his discussion of fetal therapy, paused, and made the following statement:
"There is NO diagnosis of twins. There are only monochorionic twins or dichorionic twins. This diagnosis should be written in capital red letters across the top of the patient’s chart." (Am. J. Obstet. Gynecol. 2010;203:1-2).
It could not have been better stated. It is not appropriate in obstetrical medicine to make a simple diagnosis of "twins" any longer. Early identification of whether a twin gestation involves either a monochorionic, single-placenta placentation, or a dichorionic, dual-placenta placentation is essential for accurate risk assessment and optimal antepartum management. Monochorionic pregnancies, which represent just over 20% of all twin gestations, are at much greater risk for miscarriage, congenital anomalies, growth abnormalities (including twin-to-twin transfusion syndrome), preterm birth, stillbirth, and neurodevelopmental abnormalities.
Determining this single feature – the chorionicity of the twin gestations – will thus shape a host of decisions, from the frequency of ultrasound examinations to the type of late-pregnancy surveillance and the timing of delivery.
With proper training, chorionicity can be determined with almost 100% accuracy in the first trimester, and if a patient doesn’t present in the first trimester, it still can be determined in the second trimester with an accuracy approaching 100% using a variety of ultrasound markers and parameters.
Optimizing Nutrition
I firmly believe that maximizing the mother’s nutrition is one of the most important determinants of a healthy outcome in a twin pregnancy.
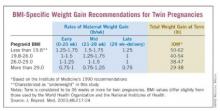
In its 2009 report titled "Weight Gain During Pregnancy: Reexamining the Guidelines," the Institute of Medicine for the first time offered body mass index–specific recommendations for women with multiple gestations. The IOM has long had recommendations for singleton pregnancies based on pregravid BMI status, but this latest report marked the first time that multiple pregnancies were addressed in such detail.
Clearly, our knowledge base has advanced. During the 1990s and 2000s, a number of investigators – most notably Barbara Luke, Sc.D., currently a professor of obstetrics, gynecology, and reproductive biology at Michigan State University, East Lansing – have published articles on the role of nutrition and weight gain in women with multiple gestations, and the relationship of these factors to pregnancy outcomes. Studies have demonstrated the critical effect that appropriate maternal weight gain and optimal nutrition have on twin fetal growth, birth weight, length of gestation, and other outcomes.