OBG Management: Many women mistake BV for a yeast infection and seek over-the-counter medication. How can physicians manage and educate this population?
Dr. Hillier: Most women who mistake BV for a yeast infection have never heard of BV. In fact, most women have been “educated” by reading articles in women’s magazines and watching television ads. Although it is important for physicians to review the symptoms of BV and other common infections with their patients, they also should advise them that symptoms are not necessarily predictive of specific diagnoses. Among women seeking care at our hospital, we find that only 1 in 4 who think they have yeast infections actually do have yeast vaginitis. When we followed women who had absolutely no evidence of yeast by culture, assessing them at 4-month intervals over a year, 25% of them reported using vaginal yeast medication. The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem in women’s health today. Personally, I would like to see much less diagnosis over the telephone and better testing for vaginal infections so that women are given the correct diagnosis.
Dr. Faro: Unfortunately, even we clinicians can look at a wet mount and miss a field that has yeast in it. We’ll look at 10 fields on each patient. Yet, when we culture that patient, it comes back positive. That raises an interesting question. Is it the yeast that’s causing their symptoms or not?
The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem.
Dr. Ledger: Most studies suggest that only 30% to 40% of women who think they have yeast, actually do. If there were a good over-the-counter test that was sensitive and specific, that would be terrific. But I don’t see that on the horizon quite yet.
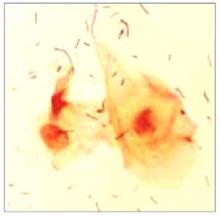
FIGURE 1 Bacterial vaginosis
Normal vaginal microflora as seen under a microscope. The flat segments depict the helpful bacteria, lactobacilli
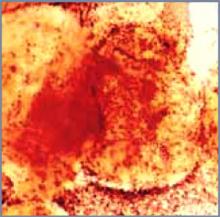
FIGURE 2 Bacterial vaginosis
An overgrowth of harmful bacteria called clue cells detected under the microscope confirms a diagnosis of BV.
Vaginal infections: detecting the difference
| BV | Yeast | Trichomoniasis | |
|---|---|---|---|
| Odor | Foul, fishy | None | Foul or fishy |
| Discharge | Thin, milky-white or gray | Thick, curdy, white | Yellow-green-gray, frothy or sticky |
| Discomfort | Itching, burning | Itching, burning | Painful urination, itch |
| Cause | Bacteria | Yeast | Parasite |
| Health risks | PID, cervicitis, cervical abnormality, endometritis, obstetric complications | None | Obstetric problems |
Dr. Faro reports no financial relationship with any companies whose products are mentioned in this article. Dr. Ledger reports receiving research grants from 3M. Dr. Hilllier reports that she has received research grants on vaginitis treatments from 3M and Pfizer, and is a consultant for Johnson & Johnson.