Appendectomy. Endometriosis of the appendix has been described in 17% of patients with bowel involvement.14 In all endometriosis surgeries, the appendix should be carefully inspected and removed if it appears abnormal. In patients who experience endometriosis-associated pelvic pain, it may be desirable to electively remove the appendix at the time of laparoscopy. This will prevent future confusion. Otherwise, emergency room physicians would have to differentiate the symptoms of chronic pelvic/abdominal pain from those of appendicitis in the event the patient presents with a complaint of pelvic pain.
Nerve interruption procedures. Two surgical procedures were designed to help reduce pain transmission in the endometriosis patient: uterosacral nerve ablation/resection and presacral neurectomy. Both involve interruption of the major efferent nerve fibers from the uterus, thus diminishing uterine and central pelvic pain. These procedures can be performed via laparoscopy or laparotomy. Unfortunately, neither has been shown to provide pain relief beyond that achieved with surgery directed against the disease itself.15-18
Outcomes
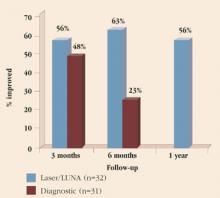
Pain relief. Although there have been many investigations of the effect of endometriosis surgery on pelvic pain, the vast majority are of low quality. No randomized, controlled trials (RCTs) have compared surgery to medical therapy, and only 1 has investigated surgery versus sham surgery. Sutton and colleagues assessed the efficacy of laser laparoscopic surgery in the treatment of pain associated with minimal, mild, or moderate endometriosis.19 They found no difference in pain at 3 months follow-up. However, by 6 months, a clear-cut advantage was seen for surgery (Figure 1). Pain relief also was maintained for at least 1 year in patients undergoing laser surgery. These patients underwent ablation of endometriosis and of the uterosacral nerve (although, as noted earlier, the latter procedure provides no additional pain relief).
Most disconcerting is the finding that only 40% of patients surgically treated for endometriosis experience pain relief as a direct result of the surgery. (The number of patients who need to be treated to reduce pain in 1 patient is 2.5.)
It remains unclear whether excision of the disease will produce better results than coagulation with the CO2 laser. Nor have the duration of pain relief and rate of reoperation been properly examined. Thus, although many surgeons feel quite strongly about the value of surgery to treat endometriosis-associated pain, there are few data to support their clinical impression of efficacy.
Fertility enhancement. Conservative surgery has been used extensively in an attempt to enhance fertility. Unfortunately, most studies on the subject are uncontrolled and of poor quality. In women who have early-stage disease, surgical therapy has resulted in pregnancy rates of 40% to 75%; in severe disease, the rates are lower, ranging from 20% to 50%.20
A meta-analysis encompassing studies from 1982 through 1994 showed that either no treatment or surgery alone is superior to medical treatment for early-stage endometriosis-associated infertility.6
A separate meta-analysis of 25 RCTs and cohort studies examined the same issue.21 It found a possible treatment benefit from laparoscopic conservative surgery, but concluded that medical treatment of the disease was ineffective.
A multicenter randomized trial (ENDOCAN) assessed the value of surgery for early-stage endometriosis in the infertile patient. In this study, 341 infertile women with minimal or mild endometriosis were randomized to diagnostic laparoscopy or resection/ablation of disease.22 They then were followed for 36 weeks. The pregnancy rates were 31% for the treated group and 18% for the diagnostic group, demonstrating a clear advantage to surgery. The data also imply that to achieve 1 additional pregnancy in 9 months, 7.7 women must be surgically treated.
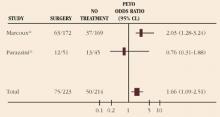
Adding confusion, a second randomized trial—this one from Italy—failed to demonstrate an improvement in fertility among those treated for early-stage endometriosis.23 Nevertheless, when the studies are combined into meta-analysis, surgical treatment of early-stage endometriosis appears to provide a significant improvement in pregnancy rates (odds ratio [OR], 1.66; 95% confidence limits [CL], 1.09-2.51) (Figure 2).
The surgical treatment of endometriosis probably enhances fertility when the disease is advanced, although no high-quality studies specifically address this issue. For early-stage disease, the data are conflicting but suggest that a small effect may exist. Further studies are needed to assess the value of surgery for this disorder.
FIGURE 1 Rate of pain relief with operative versus diagnostic laparoscopy
Adapted from: Sutton CJG, Ewen SP, Whitelaw N, Haines P. Prospective, randomized, double-blind, controlled trial of laser laparoscopy in the treatment of pelvic pain associated with minimal, mild, or moderate endometriosis. Fertil Steril. 1994;62:696.
FIGURE 2 Pregnancy rate with surgical treatment versus diagnostic laparoscopy for early-stage endometriosis
Conclusion
The role of surgery in the treatment of endometriosis is controversial. The procedure can be highly demanding technically and may involve a number of ancillary procedures besides destruction of lesions. Many questions remain unanswered. For example, we do not know the best surgical technique or ancillary procedures, or the best instruments for these procedures. While there appears to be value in treating pain and infertility, that value may be far less than anticipated. Moreover, the relative value of surgery in the treatment of endometriosis—when compared with medical therapy for pain relief or assisted reproduction for fertility enhancement—has yet to be adequately evaluated. Given this level of uncertainty and confusion, surgery should be undertaken with caution and restraint.