In pregnant women, however, the duration of the condition (pregnant and hypertensive) is finite and relatively short; as a result, maternal health benefits may not be clear. For that reason, the objective is to reduce BP to a safe level to prevent maternal cerebral complications (systolic BP below 160 mm Hg and diastolic BP below 110 mm Hg).Of course, these short-term maternal benefits must be weighed against the potential risks of fetal exposure (TABLE 3).11,12
TABLE 3
Rates of adverse pregnancy outcomes among patients with mild and severe chronic hypertension
| OUTCOME | MILD HYPERTENSION (%) | SEVERE HYPERTENSION (%) |
|---|---|---|
| Preeclampsia | 10-25 | 25-50 |
| Abruptio placentae | 0.7-1.5 | 2-5 |
| Fetal growth restriction | 8.0-15.5 | 10-20 |
| Preterm birth | 12-34.4 | 25-30 |
Low-risk disease: Avoid routine antihypertensive therapy
A limited number of randomized trials have studied the effectiveness of antihypertensive treatment in preventing adverse maternal outcomes such as superimposed preeclampsia and abruptio placentae. Here are 2 key findings:
- No demonstrable maternal benefit. Overall, there appears to be no clear benefit of antihypertensive treatment in women with mild hypertension. Indeed, the 2 largest studies had contradictory findings regarding preeclampsia,6,13 and there was no demonstrable benefit in regard to abruptio placentae.
- Antihypertensive drugs may adversely affect fetal growth. A recent meta-analysis examining antihypertensive medications in patients with mild to moderate hypertension investigated the relationship between a fall in mean arterial blood pressure and the delivery of small-for-gestational-age (SGA) infants.14 The authors concluded that antihypertensive medications induce BP drops that may adversely affect fetal growth (see FIGURE). Prior to this observation, prospective studies had shown no association between antihypertensive medications and SGA infants. (The only exception was atenolol; 3 separate studies found a relationship between treatment with atenolol and low birth weight.15-17)
Overall, maternal and perinatal data indicate that, regardless of the treatment, perinatal mortality is not improved with antihypertensive medications for mild hypertension. In fact, the indiscriminate use of such medications may have deleterious effects. Consequently, antihypertensive medications should not be used routinely in low-risk patients.18,19
Clinical care. When a woman with low-risk hypertension presents for prenatal care, it is our policy to discontinue antihypertensive medications at the first prenatal visit. Although many women will not require antihypertensive treatment during the pregnancy, careful management remains essential, as such patients can become high-risk at any time. Therapy should be initiated if her condition changes to severe hypertension (systolic BP of 180 mm Hg or more, or a diastolic blood pressure of 110 mm Hg or more).8
Low-risk women should be monitored closely for evidence of preeclampsia and fetal growth restriction. Thus, they should have a baseline ultrasound at 16 to 20 weeks’ gestation, with serial monthly ultrasounds beginning at 30 to 32 weeks to follow fetal growth. Nonstress testing or biophysical profiles are indicated in the presence of severe hypertension, preeclampsia, or abnormal fetal growth.
Patients with uncomplicated lowrisk hypertension may continue pregnancy until 40 weeks’ gestation. However, beyond 37 weeks, the presence of complications such as severe hypertension, documented growth restriction, and superimposed preeclampsia are indications for hospitalization and delivery.
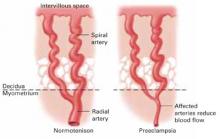
FIGURE Placental effects of hypertension
In hypertensive gravidas, placental blood flow is reduced—particularly in cases of preeclampsia. Antihypertensive therapy in low-risk women may induce blood pressure drops that further compromise fetal growth.
High-risk disease: Initiate medical therapy
Randomized, controlled trials do not exist for gravidas with high-risk hypertension—that is, women with severe hypertension or complicating factors—due to concerns about the potential adverse consequences of uncontrolled disease, such as cerebrovascular accident, congestive heart failure, and renal failure.20 It is interesting to note, however, that although controlling hypertension in such patients may help prolong pregnancy, there is no evidence that it reduces the rates of preeclampsia or abruptio placentae.20,21
Labetalol provides the added benefit of alpha-adrenergic blockade, which offers the theoretical advantage of vasodilation.
When to start treatment. For women with high-risk hypertension, hospitalization at the time of the first prenatal visit facilitates complete cardiovascular and renal evaluation, and is therefore often beneficial. If a woman has target organ damage, treatment should be initiated at a systolic BP of 140 mm Hg or a diastolicBP of 90 mm Hg. Indeed, many such women are already receiving treatment for their hypertension, in which case antihypertensive medications should be continued, though physicians should consider altering the regimen to optimize fetal safety.
Choosing the best agent. Before choosing an antihypertensive drug, review the patient’s history. If her disease was well controlled on a particular medication, that agent is probably a reasonable first choice, provided there is adequate published literature establishing the safety of her medication during pregnancy. Obviously, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II antagonists, and atenolol should be avoided because of the potential adverse effects on the fetus, including renal failure.The most commonly used medications for control of hypertension during pregnancy are listed in TABLE 4.