Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why. It may be related to decreased suturing.
DECHERNEY: Bulk is important, too—that is, the number of throws in the suture. When Vicryl (polyglactin 910) became available, we conducted a study in mice using proportionately small Vicryl plaques to determine whether this would be good a barrier (A. DeCherney, MD, unpublished data). It caused a tremendous amount of adhesion because so much foreign matter was applied.
We also did a study using human-size titanium clips in rats (A. DeCherney, MD, unpublished data). Not surprisingly, there was a lot of adhesion formation.
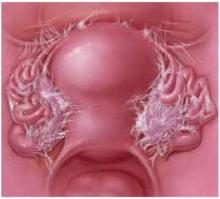
FIGURE 1 Pelvic adhesions: How they develop, problems they cause
Adhesions occur when 2 or more raw surfaces are exposed to leaking fibrin, which forms a bridge between the surfaces. Macrophages “migrate” along these bridges, depositing collagen.
The pelvis has a greater predilection for adhesions than the abdomen because of the close proximity of structures.
Although adhesions represent one of the body’s protective mechanisms, they may also cause pain or interfere with fertility, bowel function, or other processes.
Laparoscopy versus laparotomy: More adhesions in open cases?
DECHERNEY: Based on all the techniques we have learned from microsurgery—with the exception of magnification—it appears that laparoscopic procedures are less likely to cause adhesions than laparotomy. Do you agree?
PAGIDAS: I think so. As Dr. Hurd noted, a main reason is the diminished tissue handling, because there is no packing.
HURD: Multiple clinical studies have shown laparoscopy to be associated with a lower adhesion rate, although it isn’t clear why.6,7 It may be related to decreased suturing.
DECHERNEY: Less bleeding occurs because surgeons are less aggressive laparoscopically than in laparotomy.
A 15-year-old undergoes removal of a dermoid cyst, which was shelled out laparoscopically.
PAGIDAS: This case is easier because the cyst has been successfully shelled out. It is not the spill of a cyst’s contents at surgery that creates adhesions, but a chronic leak, which can occur if you do not remove the cyst in its entirety.
Once the cyst has been excised completely, I would ensure hemostasis with bipolar cautery and reapproximate the edges. I would not suture. There seems to be no clear advantage to suturing. I would use hydroflotation. Although Ringer’s lactate solution has not been shown to be effective, it is safe and has no toxicity.
DECHERNEY: Would you remove the cyst via laparotomy?
PAGIDAS: I would do it laparoscopically, using the endobag to minimize spillage, even though we know that a spill doesn’t necessarily change the outcome. If spillage does occur, I would perform copious irrigation to ensure that nothing is left behind.
HURD: My priority would be minimizing the use of power on the ovary. Studies of ovarian drilling have demonstrated that burning an ovary stimulates adhesion formation.21,22 If the dermoid cyst spills, as happens occasionally, I perform copious rinsing until no more oil is visible on the surface of the peritoneal fluid.
I also would minimize the amount of ovarian capsule that is removed. Good studies of endometriomas have shown that the more capsulate that is removed, the more adhesions. Even if the capsule looks redundant and floppy, the concern should be to achieve hemostasis with bipolar cautery and then leave it alone.
DECHERNEY: Would you use crystalloids in this case?
HURD: Yes.
SANFILIPPO: If spillage occurs, I would ensure that the patient is taken out of the Trendelenburg position. I want to emphasize the importance of thorough irrigation to eliminate any material that could produce chemical peritonitis.
DECHERNEY: Over the years, I have seen a fair number of cases of Fitz-Hugh and Curtis syndrome. You rigorously lavage a ruptured dermoid cyst, which sometimes presents with low-grade fever, but always with pain.
I’m surprised that none of you would use Interceed, since wrapping the ovary is the only thing for which it has been clearly shown to be effective. Since the cortex is relatively avascular, you don’t get a lot of bleeding. Unfortunately, it is not technically easy to wrap the ovary.
HURD: Since we do not know the effect on future fertility of changing the ovarian surface, less would seem to be better in patients this young.
I have stopped doing difficult cases laparoscopically. For example, it is rare for me to operate laparoscopically on a patient with stage IV endometriosis, at least when it comes to infertility—I might consider laparoscopy for pain.
I think case selection plays a role as well, although there are few data to back that up. It is purely clinical opinion.