Diagnostic strategy: Routine endoanal ultrasound, manometry
Our strategy is to routinely proceed with endoanal ultrasound and anal manometry to assess the anal sphincters. We may then recommend sigmoidoscopy or anoscopy to rule out mucosal lesions.
It is important to bear in mind that continence depends on multiple physiologic mechanisms and, therefore, no single diagnostic test yields positive results in all patients.
Endoanal ultrasound has significantly changed the evaluation of fecal incontinence over the last decade. In women with fecal incontinence in whom obstetric injury is suspected, 90% have sonographic evidence of injury to 1 or both sphincters.
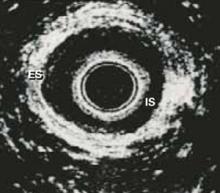
These ultrasound images show 2 discrete rings of tissue: The inner hypoechoic ring represents the internal anal sphincter and the outer hyperechoic ring represents the external anal sphincter (FIGURE 3). Disrupted continuity of these rings is consistent with structural damage to the sphincter.
Endoanal ultrasound is regarded as superior to other diagnostic methods, with an accuracy of over 90% in detecting sphincter injuries, compared to 75% for manometry, 75% for electromyography (EMG), and 50% for clinical assessment.7,8 It is the simplest and least-invasive test to assess the structural integrity of the anal sphincters.
It can also serve as a screening tool to detect occult sphincter injury following vaginal delivery, thus identifying women at high risk for future incontinence. Women with transient stool or gas incontinence following vaginal delivery may be candidates for screening endoanal ultrasound for further evaluation.
- Where endoanal ultrasound is unavailable, transperineal ultrasound may be an alternative option.
Anorectal manometry can detect functional weakness of sphincters that are anatomically intact by measuring sensation and squeeze pressures. Patients with intact sphincters but abnormal anal manometry findings may benefit from physical therapy and biofeedback aimed at increasing muscular function by stimulating the neuromuscular feedback loop.
During manometry, the physician assesses maximum resting and squeeze pressures of the anal canal, the rectoanal inhibitory reflex, rectal sensation, and rectal compliance using either water-perfused catheters, solid-state microtransducers, or air-or water-filled balloons. Normal values vary widely among institutions and are poorly standardized.
Decreased resting pressure suggests isolated internal anal sphincter injury; decreased squeeze pressure suggests external anal sphincter injury. Of all parameters, maximum squeeze pressure has the greatest sensitivity and specificity at a cut-off of 60 mm Hg in women.9
Rectal sensory testing also is useful in identifying patients who may benefit from biofeedback therapy, and can detect afferent nerve injury as a contributing cause of incontinence. Biofeedback is unlikely to be useful in patients with a poor or absent sensation. In addition, for patients already involved in biofeedback, the test can assess rectal response to training and indicate rectal irritability or poor compliance.
Rectal sensation is assessed by inflating a balloon in the rectum and recording the smallest volume of rectal distention for first detectable sensation (rectal sensory threshold), sensory urgency, and pain (maximum tolerable volume).
Ancillary tests are of limited benefit as screening tools, but may have utility in special circumstances.
- Electromyography of the external anal sphincter and the pelvic floor muscles—traditionally performed using needle electrodes or surface electrodes—is helpful in delineating areas of sphincter injury by mapping the sphincter. However, much of this information is now obtained accurately by endoanal ultrasound, which has replaced needle EMG for most clinicians. Surface EMG is still useful for evaluating sphincter function and in biofeedback training.
- Defecography involves imaging the rectum after filling it with contrast material, and then observing the process, rate, and completeness of rectal evacuation using fluoroscopy. Its usefulness in the evaluation of fecal incontinence is limited to cases of rectal prolapse and for the diagnosis of rectocele and enterocele.
- Investigational: Pudendal nerve testing. This test uses an electrode to measure pudendal nerve conduction time, known as pudendal nerve terminal motor latency (PNTML)—thus allowing further investigation for nerve injury.
- Normal PNTML value is 2.2 milliseconds.
- A value between 2.2 and 2.6 milliseconds indicates probable nerve damage.
- A value of 2.6 milliseconds or greater confirms nerve damage.
Clinical use of PNTML is controversial; it helps diagnose nerve injury, but is currently reserved for investigational purposes.10
FIGURE 3 Endoanal ultrasound
Disruption of continuity of the inner hypoechoic ring (IS, internal sphincter) and the outer hyperechoic ring (ES, external sphincter) on endoanal ultrasound is consistent with structural damage to the sphincter. This image shows normal anatomy.
Mainstays: Nonsurgical treatments
The general principles of treatment are to identify the underlying cause of incontinence and direct therapy based on these findings. Since much of the disability in these patients is psychological, a supportive medical team is essential. Patient educational books, advice on the use of continent aides, and perianal skin care also are crucial.