JUDY’S CASE
“WHAT’S MY RISK?”
At her periodic gynecologic exam, Judy, a 58-year-old white woman, expresses concern about her heart health in light of her 62-year-old sister’s recent heart attack. Further questioning reveals that her father died of a heart attack at age 56, and her brother, 52, has high blood pressure and adult-onset diabetes.
Judy has not experienced any symptoms of cardiovascular disease, such as chest pain or tightness with exertion, and she doesn’t smoke. The last time her cholesterol was checked was about 15 years earlier, at which time it was “OK.” She admits she is not very physically active and has gained about 30 lb over the past 10 years. Her vital signs and physical exam are entirely normal except for borderline high blood pressure at 140/90 mm Hg, weight of 170 lb (height: 68 inches), and a waist circumference of 37 inches.
What is her cardiovascular risk?
Judy has physical findings suggestive of metabolic syndrome in addition to the significant family history of cardiovascular disease (CVD). Although her current risk of a cardiac event appears to be low, she is likely to deteriorate if the hypertension and excess body weight are not addressed.
To predict her level of risk more precisely, the physician asks Judy to return in 2 weeks for a blood pressure recheck, and instructs her to perform additional readings on her own. The clinician also refers Judy for a fasting lipid panel and blood glucose level.
In women, CVD is especially lethal
Contrary to earlier assumptions, CVD now appears to be more lethal in women than in men and warrants aggressive efforts to prevent it and manage risk factors (FIGURE). This article focuses on improving high-density lipoprotein (HDL) cholesterol, a key factor in women at risk.
This approach differs slightly from the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines, which target low-density lipoprotein (LDL) cholesterol as the primary lipid risk factor for intervention.1
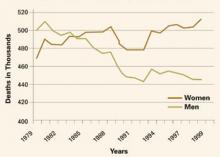
FIGURE Women surpass men in CVD deaths
Over the past 25 years, the trend in deaths attributable to cardiovascular disease has been upward for women, while it is shifting downward for men.
Why focus on HDL?
Improvement in HDL is the strongest predictor of reduced risk for cardiac events. So says an analysis of 17 major lipid intervention trials between 1987 and 2003 (n = 44,170).2
Another study3 demonstrated that HDL cholesterol is the stronger predictor of CVD risk in women. In addition, several large observational studies have shown that increasing HDL cholesterol by 1 mg/dL in men reduces CVD risk by 2%, whereas increasing HDL in women by 1 mg/dL decreases CVD risk by 3%.4
Higher HDL levels may explain later onset of CVD in women. The advantage that women have over men in CVD risk prior to menopause seems to be at least partly due to their higher levels of HDL cholesterol: The average HDL level in women is 56 mg/dL, versus 46 mg/dL in men. This advantage begins to disappear after menopause, presumably because of changes in hormone levels and decreasing HDL-2 cholesterol, the most cardioprotective HDL fraction.
Other reasons to focus on HDL. In addition to the increased CVD risk associated with menopause, women of all ages in the United States have an increasing tendency—at almost epidemic rates—toward obesity and metabolic syndrome, which are known CVD risk factors.5 The dyslipidemia seen with those conditions is characterized by low HDL cholesterol and high triglycerides. Thus, maintaining healthy HDL levels is clearly an important goal for overall cardiovascular health, especially in women.
In addition, HDL is the key lipoprotein associated with reverse cholesterol transport, the process of carrying excess cholesterol from peripheral tissues to the liver for catabolism.
JUDY’S CASE
METABOLIC SYNDROME CONFIRMED
At her return visit, Judy’s blood pressure remains 140/90 mm Hg, with outside readings ranging from 135 to 145 mm Hg systolic and 85 to 95 mm Hg diastolic. Her laboratory tests reveal fasting blood glucose of 115 mg/dL, total cholesterol of 220 mg/dL, LDL cholesterol of 120 mg/dL, HDL cholesterol of 35 mg/dL, and triglycerides of 300 mg/dL.