4. Keep molding in mind
Some (up to +2) occipito-parietal molding may be normal in the late stages of delivery (ie, the occipital bone slips under the 2 parietal bones, but can be easily reduced), but severe parieto-parieto molding is never normal and should be interpreted as a sign of relative or absolute cephalopelvic disproportion. FIGURE 1 shows a classification system for molding.
FIGURE 1 How to characterize the degree of molding
Excessive molding may lead to tears in dura and underlying vessels.
Traction plus severe molding may increase the risk of intracranial injury
The most frequent causes of molding are asynclitism and deflexion of the head, commonly seen in occiput posterior and transverse positions. Correction of the asynclitism and malposition may correct the molding and allow safe vaginal delivery. Traction on a head with severe molding may increase the risk of intracranial injury.
Using maximum likelihood logistic regression analyses, Knight and colleagues6 demonstrated that the factor of greatest importance in determining whether a case would be allocated to engaged versus unengaged groups was molding (odds ratio 2.17; 95% confidence intervals 0.75–6.27). The authors concluded that when abdominal and vaginal assessments produce different findings, the major factor responsible is molding. They noted that data derived from vaginal examination alone may be misleading when molding is present.
The rule of 3’s
With the fetus in an occiput anterior position, determine the number of fifths of the fetal head that can be palpated above the pelvic brim abdominally, add it to the degree of molding palpated vaginally, and avoid operative vaginal delivery if the sum is 3 or higher (FIGURE 2).7
FIGURE 2 Abdominopelvic assessment using the rule of 3’s
If the sum of the number of fifths of the fetal head palpated above the pelvic brim abdominally and the degree of molding palpated vaginally equals or exceeds 3, operative vaginal delivery is unlikely to be successful.For example, if two fifths (~4 cm) of the fetal head is palpated above the maternal pubic symphysis, and there is already +1 of parieto-parieto molding, significant cephalopelvic disproportion is likely and operative vaginal delivery will probably fail, with an increased risk of fetal and maternal damage. Obviously, if three fifths or more of the fetal head is palpated abdominally, the head is not engaged and operative vaginal delivery is contraindicated, regardless of whether the scalp is felt at or below the ischial spines.
Knowledge of fetal head diameters is useful
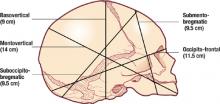
Using measurements of fetal head diameters (FIGURE 3), it is easy to see why a vertex presentation in an occiput anterior position (presenting diameter=suboccipitobregmatic diameter=9.5 cm) will deliver more easily than a baby in a deflexed occiput posterior position (presenting diameter=occipitofrontal diameter ≥ 11.5 cm). The presenting diameter of a brow presentation will never negotiate a normally proportioned female pelvis, whereas that of a mentum anterior face presentation is clearly adequate for a vaginal delivery if all other factors are favorable.
FIGURE 3 Know the basic term fetal head diameters
Depending on the presentation, the fetal head will deliver easily, as in occiput anterior position, when the presenting diameter is 9.5 cm, or with difficulty, as when the presenting diameter is 11.5 cm or more.
5. Be aware of fetal head position throughout labor
Early documentation of fetal head position during labor may help tremendously when decisions regarding the mode of delivery have to be made in a hurry. If one is aware that the head has been persistently in a deflexed occiput posterior position (or a transverse position) throughout the labor, a prolongation or arrest of descent can be explained by progressive deflexion of the head and increasing presenting diameters (or deep transverse arrest, as the case may be).
In such a case, if sudden fetal decompensation necessitates emergent delivery, operative vaginal delivery is a much less viable option than it would be with a well-flexed occiput anterior position at the same station.
When there is knowledge of a fetal malposition, cesarean section may be the wisest choice in an emergency, even if the fetal head is at an appropriate station, unless the operator has the requisite skills at operative vaginal delivery and is certain of a high chance of a successful outcome.
6. Have a valid indication
Operative vaginal delivery should not proceed without a valid indication8 that conforms to accepted guidelines.
Consider the pathology underlying the indication
For example, although maternal exhaustion is clearly a valid indication for operative vaginal delivery, it is important to examine the underlying reason for the exhaustion. A diabetic mother who is known to have a large-for-gestational-age infant, who has a prolonged active phase (8 hours) and is exhausted after 3 hours of excellent pushing with adequate contractions, may appear to have, on the surface, a valid indication—but clearly this situation calls for extreme caution. The size of the infant and the lack of progress suggest at the least the potential for cephalopelvic disproportion.