Treatment of thyroid storm begins with stabilization of the patient, followed by initiation of a stepwise management approach (FIGURE 2).
FIGURE 2 Management of thyroid storm
Aggressive management of thyroid storm is indicated, following a stepwise approach. Each medication used to treat thyroid storm plays a specific role in suppressing thyroid function. Propylthiouracil (PTU) blocks additional synthesis of thyroid hormone and inhibits the conversion of thyroxine (T4) to triiodothyronine (T3). Methimazole blocks additional synthesis of thyroid hormones. Saturated solution of potassium iodide (SSKI), Lugol’s solution, and sodium iodide block the release of thyroid hormone from the gland. Dexamethasone is used to decrease thyroid hormone release and peripheral conversion of T4 to T3. Propranolol is used to treat maternal tachycardia by inhibiting the adrenergic effects of excessive thyroid hormones. Finally, phenobarbital is used to treat maternal agitation and restlessness caused by the increased catabolism of thyroid hormones.
SOURCE: Adapted from ACOG.2
Treatment of hyperthyroidism in pregnancy
Two medications are available to treat hyperthyroidism in pregnancy: propylthiouracil (PTU) and methimazole. These medications are known as thioamides.1,2
PTU blocks the oxidation of iodine in the thyroid gland, thereby preventing the synthesis of T4 and T3. The initial dosage for hyperthyroid women who are not pregnant is usually 300 to 450 mg/day in three divided doses every 8 hours, and this dosing strategy can also be applied to the pregnant patient. Maintenance therapy is usually achieved with 100 to 150 mg/day in divided doses every 8 to 12 hours.9
Methimazole works by blocking the organification of iodide, which decreases thyroid hormone production. The usual dosing, given in three divided doses every 8 hours, is 15 mg/day for mild hyperthyroidism, 30 to 40 mg/day for moderately severe hyperthyroidism, and 60 mg/day for severe hyperthyroidism. Maintenance therapy with methimazole is usually given at a dosage of 5 to 15 mg/day.9
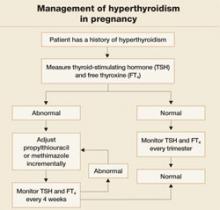
In the past, PTU was considered the drug of choice for treatment of hyperthyroidism in pregnancy because clinicians believed it crossed the placenta to a lesser degree than did methimazole, and because methimazole was associated with fetal esophageal and choanal atresia and fetal cutis aplasia (congenital skin defect of the scalp).1,2 Available evidence does not, however, support these conclusions.8,10 Whatever medication regimen you choose, thyroid function should be monitored 1) every 4 weeks until TSH and FT4 levels are within normal limits and 2) every trimester thereafter. FIGURE 3 presents an algorithm for managing hyperthyroidism in pregnancy.
FIGURE 3 Management of hyperthyroidism in pregnancy
CASE Resolved
The patient in thyroid storm described at the beginning of this article requires aggressive management, as outlined in the algorithm in FIGURE 2. As her symptoms diminish, fetal tachycardia resolves. The patient’s FT4 level begins to decline, consistent with appropriate treatment, and she is discharged home and instructed to continue PTU and labetalol and to follow up at the endocrinology and high-risk obstetrics clinics as soon as possible.
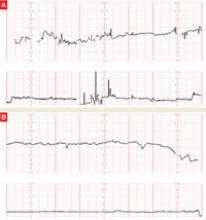
The patient does not follow this advice. Consequently, she presents at 33 5/7 weeks in a hypertensive crisis, with symptoms similar to those she first exhibited plus acute pulmonary edema. Fetal heart rate is initially in the 130s, with good variability and occasional decelerations (FIGURE 4A), but decelerations then become worse (FIGURE 4B) and emergency cesarean section is performed.
A male infant is delivered, weighing 2,390 g. Apgar scores are 0 at 1 minute and 9 at 5 minutes. A 25% placental abruption is noted at the time of delivery.
Mother and fetus are stabilized and discharged.
FIGURE 4 Weakening fetal status in a mother who is in thyroid storm
Fetal heart rate is initially in the 130s with good variability and occasional decelerations (A), but then deteriorates, with increasing decelerations (B), an indication for immediate delivery.